Biomarker Panel Evaluated for Primary Hyperoxaluria Patients
By LabMedica International staff writers
Posted on 27 Apr 2020
Primary hyperoxaluria (PH) is a group of autosomal recessive disorders characterized by recurrent urinary stones and nephrocalcinosis. Roughly half of PH patients present with advanced chronic kidney disease (CKD) at the time of diagnosis.Posted on 27 Apr 2020
Three forms of PH have been recognized based on the underlying genetic defects. Mutations in the AGXT, GRHPR, and HOGA1 genes cause primary hyperoxaluria types 1, 2, and 3, respectively. The main biochemical defect in PH is overproduction of oxalate due to enzyme deficiencies, primarily in the liver. The excess oxalate must then be excreted by the kidney. In the kidney oxalate can combine with calcium within renal tubules leading to nephrocalcinosis and kidney stones.
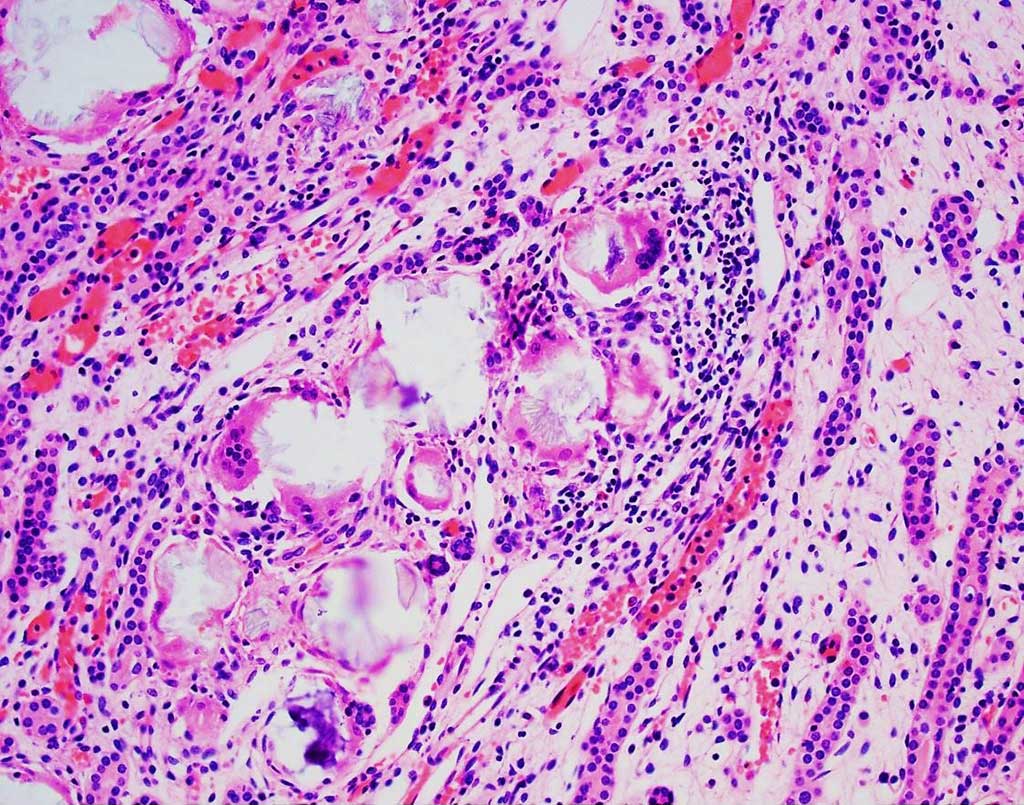
Image: Histology of multinucleated giant cells engulfing calcium oxalate crystals from a patient with type 1 primary hyperoxaluria (Photo courtesy of Jonathan E. Zuckerman, MD, PhD).
Nephrologists and their colleagues from the Mayo Clinic (Rochester, MN, USA) enrolled 30 PH patients who had one or more biobanked urine specimens and no prior history of end stage renal disease (ESRD) or organ transplantation. A cohort of 47 non-stone forming adults in good general health without kidney disease or diabetes (22 women, 25 men, ages ranging from 23 to 77 years) who completed 24-hour urine collections on a free choice diet served as the adult control group to establish an adult reference range for the urine biomarkers.
The scientists used a panel of biomarkers that reflect different nephron sites and potential mechanisms of injury (clusterin, neutrophil gelatinase-associated lipocalin (NGAL), 8-isoprostane (8IP), monocyte-chemoattractant protein 1 (MCP-1), liver-type fatty acid binding protein (L-FABP), heart-type fatty acid binding protein (H-FABP), and osteopontin (OPN) were measured in 114 urine specimens from 30 PH patients over multiple visits. Generalized estimating equations were used to assess associations between biomarkers and 24 hour urine excretions, calculated proximal tubular oxalate concentration (PTOx), and estimated glomerular filtration rate (eGFR).
The team reported that mean (±SD) age at first visit was 19.5 ± 16.6 years with an estimated glomerular filtration rate (eGFR) of 68.4 ± 21.0 mL/min/1.73m2. After adjustment for age, sex, and eGFR, a higher urine MCP-1 concentration as measured by Quantikine Human chemokine (C-C motif) ligand 2/ monocyte chemoattractant protein-1 (CCL2/MCP1) kit (R&D Systems, Minneapolis, MN, USA) and MCP-1/creatinine ratio was positively associated with calcium oxalate supersaturation (CaOx SS). Higher urine NGAL and NGAL/creatinine as well as OPN and OPN/creatinine were associated with higher eGFR. 8IP was negatively associated with PTOx and urinary Ox, but positively associated with CaOx SS.
The authors concluded that although the mechanisms are not entirely clear, CaOx crystallization in renal tubules has been considered as one of the critical therapeutic targets in the development of new therapeutic approach to treat PH. The association between urine level of MCP-1 and CaOx crystallization may suggest urine MCP-1 could be used as a marker to assist the evaluation for the effectiveness of treatments in PH patients. In addition, this association may suggest that MCP-1 signaling pathway might be in involved in the etiology of renal damage in PH. The study was published on April 15, 2020 in the journal BMC Nephrology.
Related Links:
Mayo Clinic
R&D Systems