Next-Generation Sequencing Detects Residual Disease in Acute Lymphoblastic Leukemia
By LabMedica International staff writers
Posted on 24 Dec 2020
The use of next-generation sequencing (NGS) to detect residual disease in acute lymphoblastic leukemia (ALL) patients after treatment can better gauge their risk of relapse and overall survival than multiparameter flow cytometry.Posted on 24 Dec 2020
Although flow cytometry is commonly used to assess residual disease in leukemia patients, some patients deemed to be negative for measurable residual disease (MRD-negative) at remission by this method, later relapse. Scientists wanted to determine if using a more sensitive test to measure residual disease, like NGS, would benefit ALL patients.
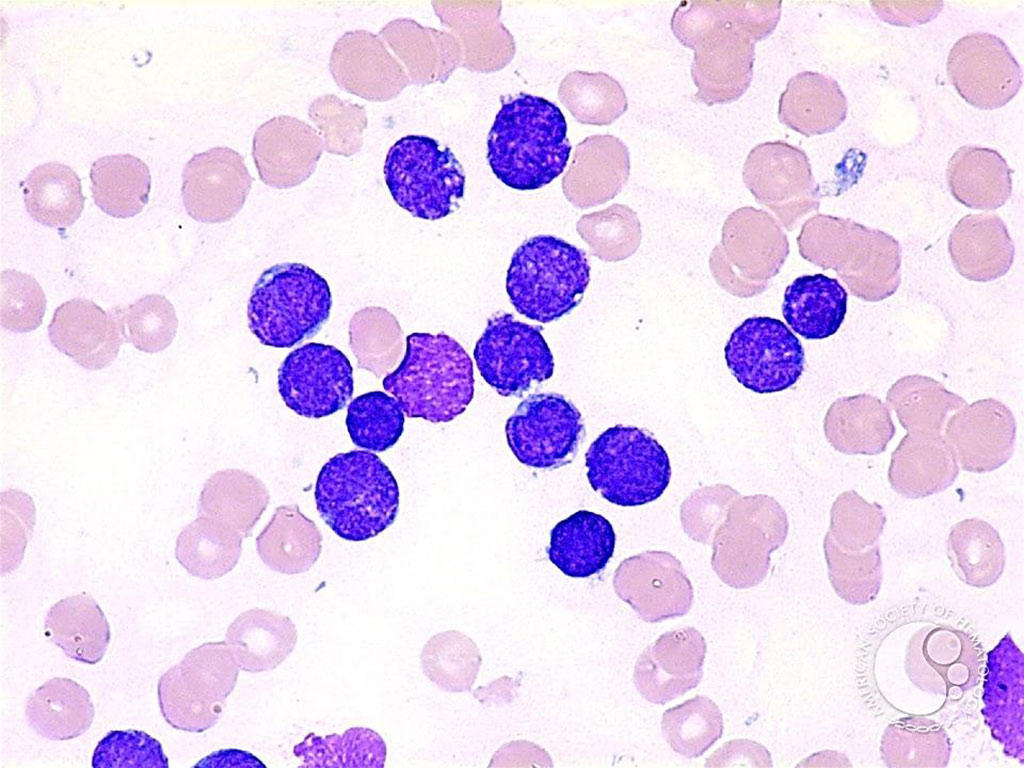
Image: Acute Lymphoblastic Leukemia: lymphoblasts appear small with a thin rim of cytoplasm (Photo courtesy of Peter Maslak MD).
Hematologists and Oncologists at The University of Texas MD Anderson Cancer Center (Houston, TX, USA) retrospectively analyzed data from 67 previously untreated Philadelphia chromosome-negative ALL patients who had received either a standard-intensity chemotherapy regimen or lower-intensity regimen. The team tested 109 bone marrow samples provided by these patients by both flow cytometry and NGS to determine MRD status.
The scientists used the ClonoSEQ assay developed by Adaptive Biotechnologies (Seattle, WA, USA) which was the first next-generation sequencing (NGS) test approved for measuring residual disease in ALL patients. Prior to that test being approved, flow cytometry and PCR-based assays were the standard and could measure residual disease down to 1 in 10,000 or 1 in 100,000 cells. The NGS assays, however, can measure residual disease down to 1 in 1 million cells.
In the analysis of the 84 samples that were MRD-negative by flow cytometry, the NGS test found 38% of those were MRD-positive, meaning leukemia remained in these samples that was below the level of detection from flow cytometry. Overall, when samples across patient subgroups were tested with NGS, they were less likely to achieve MRD-negative status than when tested with flow cytometry. The investigators broke up the study cohort into two subgroups by the type of frontline chemotherapy patients received, either a standard chemotherapy-based regimen (involving cyclophosphamide/vincristine/doxorubicin/dexamethasone), called hyper-CVAD, or a lower-intensity version of the regimen, called hyper-CVD.
At the time of remission, 61% of patients who were treated with hyper-CVAD were deemed MRD-negative by flow cytometry, but only 32% in this subgroup were MRD-negative by NGS. Patients who received the lower intensity hyper-CVD regimen saw slightly better results by both methods, with 74% reaching MRD-negative status by flow cytometry and 46% by NGS. The number of patients who relapsed within five years after achieving MRD-negative status was higher among patients tested with flow cytometry (27%) than those with NGS (8%). Only one of the 14 ALL patients who were deemed MRD-negative by NGS later relapsed.
Nicholas J. Short, MD, an assistant professor and senior author of the study, said, “It will always be somewhat complementary, even with the more sensitive flow assay, to use two different types of MRD assays that are looking at slightly different things, for example, using flow cytometry for other specific markers and an NGS panel looking at these rearrangements.”
The authors concluded that early assessment of MRD using an ultrasensitive NGS assay can identify patients with ALL who have a very low risk of relapse and excellent long-term survival. Prospective studies are warranted to assess whether de-intensification of therapy is feasible for this favorable-risk group of patients who rapidly achieve MRDneg remission. The study was presented at the virtual 62nd American Society for Hematology's annual meeting held December 5-8, 2020.
Related Links:
The University of Texas MD Anderson Cancer Center
Adaptive Biotechnologies














