Genetic Test Helps Patients Avoid Unnecessary Thyroid Surgery
|
By LabMedica International staff writers Posted on 19 Nov 2018 |
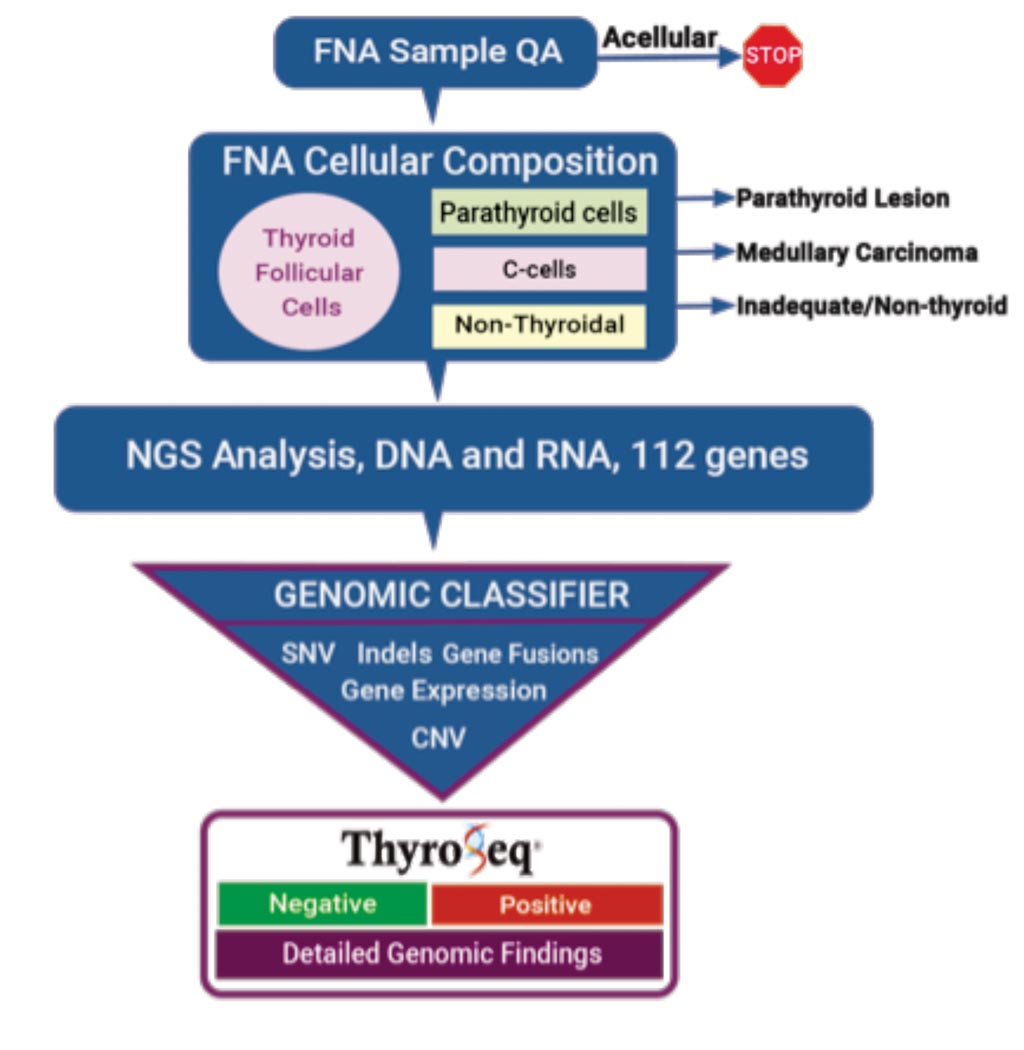
Image: A diagram workflow of the ThyroSeq Genomic Classifier assay to determine preoperative thyroid cancer status (Photo courtesy of ThyroSeq).
A genetic test has been developed that can help avoid costly diagnostic surgery that involves removing one or both lobes of the thyroid gland, by reliably distinguishing between benign and cancerous thyroid nodules using a very small sample of cells.
Thyroid nodules are common, and approximately 600,000 patients with nodules undergo a fine needle aspiration (FNA) biopsy every year, where cells are extracted from the nodule and examined to determine whether it is benign or cancerous. While the biopsy test is mostly accurate, it returns an indeterminate finding in approximately one-in-four to -five cases, which forces patients to undergo either a repeat FNA, or diagnostic surgery where at least half of the patients' thyroid is removed for further assessment.
A large team of scientists collaborating with the University of Pittsburgh School of Medicine (Pittsburgh, PA, USA) carried out a prospective cohort study and recruited 782 patients with 1,013 thyroid nodules clinically evaluated at 10 sites, nine in the USA and one in Singapore, between January 2015 and December 2016. Fine-needle aspiration (FNAs) samples were collected for molecular analysis by either rinsing the residual material in the aspiration needle from all passes or collecting a dedicated pass into a preservative solution tube.
The team used the ThyroSeq v3 Genomic Classifier (GC) (ThyroSeq, Oakland, PA, USA) which is a targeted next-generation sequencing test that interrogates selected regions of 112 thyroid cancer-related genes for point mutations, insertions/deletions, gene fusions, copy number alterations, or gene expression alterations. The test is designed to diagnose all types of thyroid cancer, including Hurthle cell cancer, as well as medullary carcinoma and parathyroid lesions. The genomic classifier was applied to assign a value to each detected genetic alteration based on the strength of association with malignancy: 0 (no association with cancer), 1 (low cancer probability), or 2 (high cancer probability).
The team reported that of the 286 cytological indeterminate nodules, 206 (72%) were benign, 69 (24%) malignant, and 11 (4%) noninvasive follicular thyroid neoplasms with papillary-like nuclei (NIFTP). A total of 257 (90%) nodules (154 Bethesda III, 93 Bethesda IV, and 10 Bethesda V) had informative GC analysis, with 61% classified as negative and 39% as positive. In Bethesda III and IV nodules combined, the test demonstrated 94% sensitivity and 82% specificity. The observed 3% false-negative rate was similar to that of benign cytology, and the missed cancers were all low-risk tumors. Among nodules testing positive, specific groups of genetic alterations had cancer probabilities varying from 59% to 100%.
David Steward, MD, a professor of otolaryngology and first author of the study, said, “Beyond simply differentiating benign and malignant nodules, the study shows that ThyroSeq also provides a detailed genetic profile of the positive nodules. Since thyroid cancer is known to progress differently based on the mutation involved, ThyroSeq potentially allows physicians to employ a precision medicine approach, modifying treatment for each patient based on the mutations present.” The study was published on November 8, 2018, in the journal JAMA Oncology.
Related Links:
University of Pittsburgh School of Medicine
ThyroSeq
Thyroid nodules are common, and approximately 600,000 patients with nodules undergo a fine needle aspiration (FNA) biopsy every year, where cells are extracted from the nodule and examined to determine whether it is benign or cancerous. While the biopsy test is mostly accurate, it returns an indeterminate finding in approximately one-in-four to -five cases, which forces patients to undergo either a repeat FNA, or diagnostic surgery where at least half of the patients' thyroid is removed for further assessment.
A large team of scientists collaborating with the University of Pittsburgh School of Medicine (Pittsburgh, PA, USA) carried out a prospective cohort study and recruited 782 patients with 1,013 thyroid nodules clinically evaluated at 10 sites, nine in the USA and one in Singapore, between January 2015 and December 2016. Fine-needle aspiration (FNAs) samples were collected for molecular analysis by either rinsing the residual material in the aspiration needle from all passes or collecting a dedicated pass into a preservative solution tube.
The team used the ThyroSeq v3 Genomic Classifier (GC) (ThyroSeq, Oakland, PA, USA) which is a targeted next-generation sequencing test that interrogates selected regions of 112 thyroid cancer-related genes for point mutations, insertions/deletions, gene fusions, copy number alterations, or gene expression alterations. The test is designed to diagnose all types of thyroid cancer, including Hurthle cell cancer, as well as medullary carcinoma and parathyroid lesions. The genomic classifier was applied to assign a value to each detected genetic alteration based on the strength of association with malignancy: 0 (no association with cancer), 1 (low cancer probability), or 2 (high cancer probability).
The team reported that of the 286 cytological indeterminate nodules, 206 (72%) were benign, 69 (24%) malignant, and 11 (4%) noninvasive follicular thyroid neoplasms with papillary-like nuclei (NIFTP). A total of 257 (90%) nodules (154 Bethesda III, 93 Bethesda IV, and 10 Bethesda V) had informative GC analysis, with 61% classified as negative and 39% as positive. In Bethesda III and IV nodules combined, the test demonstrated 94% sensitivity and 82% specificity. The observed 3% false-negative rate was similar to that of benign cytology, and the missed cancers were all low-risk tumors. Among nodules testing positive, specific groups of genetic alterations had cancer probabilities varying from 59% to 100%.
David Steward, MD, a professor of otolaryngology and first author of the study, said, “Beyond simply differentiating benign and malignant nodules, the study shows that ThyroSeq also provides a detailed genetic profile of the positive nodules. Since thyroid cancer is known to progress differently based on the mutation involved, ThyroSeq potentially allows physicians to employ a precision medicine approach, modifying treatment for each patient based on the mutations present.” The study was published on November 8, 2018, in the journal JAMA Oncology.
Related Links:
University of Pittsburgh School of Medicine
ThyroSeq
Latest Molecular Diagnostics News
- Blood Proteins Could Warn of Cancer Seven Years before Diagnosis
- New DNA Origami Technique to Advance Disease Diagnosis
- Ultrasound-Aided Blood Testing Detects Cancer Biomarkers from Cells
- New Respiratory Syndromic Testing Panel Provides Fast and Accurate Results
- New Synthetic Biomarker Technology Differentiates Between Prior Zika and Dengue Infections
- Novel Biomarkers to Improve Diagnosis of Renal Cell Carcinoma Subtypes
- RNA-Powered Molecular Test to Help Combat Early-Age Onset Colorectal Cancer
- Advanced Blood Test to Spot Alzheimer's Before Progression to Dementia
- Multi-Omic Noninvasive Urine-Based DNA Test to Improve Bladder Cancer Detection
- First of Its Kind NGS Assay for Precise Detection of BCR::ABL1 Fusion Gene to Enable Personalized Leukemia Treatment
- Urine Test to Revolutionize Lyme Disease Testing
- Simple Blood Test Could Enable First Quantitative Assessments for Future Cerebrovascular Disease
- New Genetic Testing Procedure Combined With Ultrasound Detects High Cardiovascular Risk
- Blood Samples Enhance B-Cell Lymphoma Diagnostics and Prognosis
- Blood Test Predicts Knee Osteoarthritis Eight Years Before Signs Appears On X-Rays
- Blood Test Accurately Predicts Lung Cancer Risk and Reduces Need for Scans
Channels
Clinical Chemistry
view channel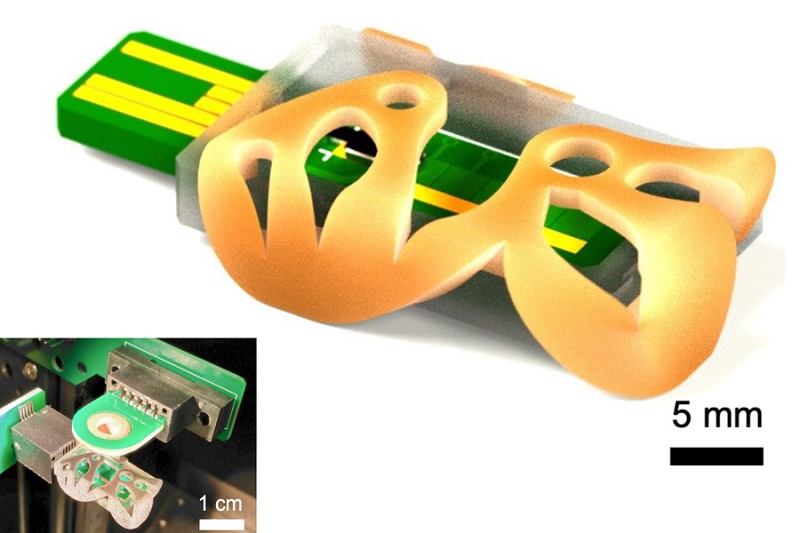
3D Printed Point-Of-Care Mass Spectrometer Outperforms State-Of-The-Art Models
Mass spectrometry is a precise technique for identifying the chemical components of a sample and has significant potential for monitoring chronic illness health states, such as measuring hormone levels... Read more.jpg)
POC Biomedical Test Spins Water Droplet Using Sound Waves for Cancer Detection
Exosomes, tiny cellular bioparticles carrying a specific set of proteins, lipids, and genetic materials, play a crucial role in cell communication and hold promise for non-invasive diagnostics.... Read more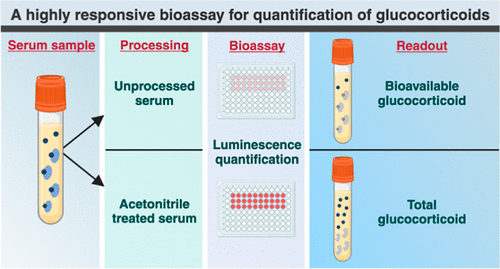
Highly Reliable Cell-Based Assay Enables Accurate Diagnosis of Endocrine Diseases
The conventional methods for measuring free cortisol, the body's stress hormone, from blood or saliva are quite demanding and require sample processing. The most common method, therefore, involves collecting... Read moreMolecular Diagnostics
view channelBlood Proteins Could Warn of Cancer Seven Years before Diagnosis
Two studies have identified proteins in the blood that could potentially alert individuals to the presence of cancer more than seven years before the disease is clinically diagnosed. Researchers found... Read moreUltrasound-Aided Blood Testing Detects Cancer Biomarkers from Cells
Ultrasound imaging serves as a noninvasive method to locate and monitor cancerous tumors effectively. However, crucial details about the cancer, such as the specific types of cells and genetic mutations... Read moreHematology
view channel
Next Generation Instrument Screens for Hemoglobin Disorders in Newborns
Hemoglobinopathies, the most widespread inherited conditions globally, affect about 7% of the population as carriers, with 2.7% of newborns being born with these conditions. The spectrum of clinical manifestations... Read more
First 4-in-1 Nucleic Acid Test for Arbovirus Screening to Reduce Risk of Transfusion-Transmitted Infections
Arboviruses represent an emerging global health threat, exacerbated by climate change and increased international travel that is facilitating their spread across new regions. Chikungunya, dengue, West... Read more
POC Finger-Prick Blood Test Determines Risk of Neutropenic Sepsis in Patients Undergoing Chemotherapy
Neutropenia, a decrease in neutrophils (a type of white blood cell crucial for fighting infections), is a frequent side effect of certain cancer treatments. This condition elevates the risk of infections,... Read more
First Affordable and Rapid Test for Beta Thalassemia Demonstrates 99% Diagnostic Accuracy
Hemoglobin disorders rank as some of the most prevalent monogenic diseases globally. Among various hemoglobin disorders, beta thalassemia, a hereditary blood disorder, affects about 1.5% of the world's... Read moreImmunology
view channel.jpg)
AI Predicts Tumor-Killing Cells with High Accuracy
Cellular immunotherapy involves extracting immune cells from a patient's tumor, potentially enhancing their cancer-fighting capabilities through engineering, and then expanding and reintroducing them into the body.... Read more
Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
Transplanted organs constantly face the risk of being rejected by the recipient's immune system which differentiates self from non-self using T cells and B cells. T cells are commonly associated with acute... Read more
AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
Current strategies for matching cancer patients with specific treatments often depend on bulk sequencing of tumor DNA and RNA, which provides an average profile from all cells within a tumor sample.... Read more
Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
Cancer treatment typically adheres to a standard of care—established, statistically validated regimens that are effective for the majority of patients. However, the disease’s inherent variability means... Read moreMicrobiology
view channel
Integrated Solution Ushers New Era of Automated Tuberculosis Testing
Tuberculosis (TB) is responsible for 1.3 million deaths every year, positioning it as one of the top killers globally due to a single infectious agent. In 2022, around 10.6 million people were diagnosed... Read more
Automated Sepsis Test System Enables Rapid Diagnosis for Patients with Severe Bloodstream Infections
Sepsis affects up to 50 million people globally each year, with bacteraemia, formerly known as blood poisoning, being a major cause. In the United States alone, approximately two million individuals are... Read moreEnhanced Rapid Syndromic Molecular Diagnostic Solution Detects Broad Range of Infectious Diseases
GenMark Diagnostics (Carlsbad, CA, USA), a member of the Roche Group (Basel, Switzerland), has rebranded its ePlex® system as the cobas eplex system. This rebranding under the globally renowned cobas name... Read more
Clinical Decision Support Software a Game-Changer in Antimicrobial Resistance Battle
Antimicrobial resistance (AMR) is a serious global public health concern that claims millions of lives every year. It primarily results from the inappropriate and excessive use of antibiotics, which reduces... Read moreTechnology
view channel
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more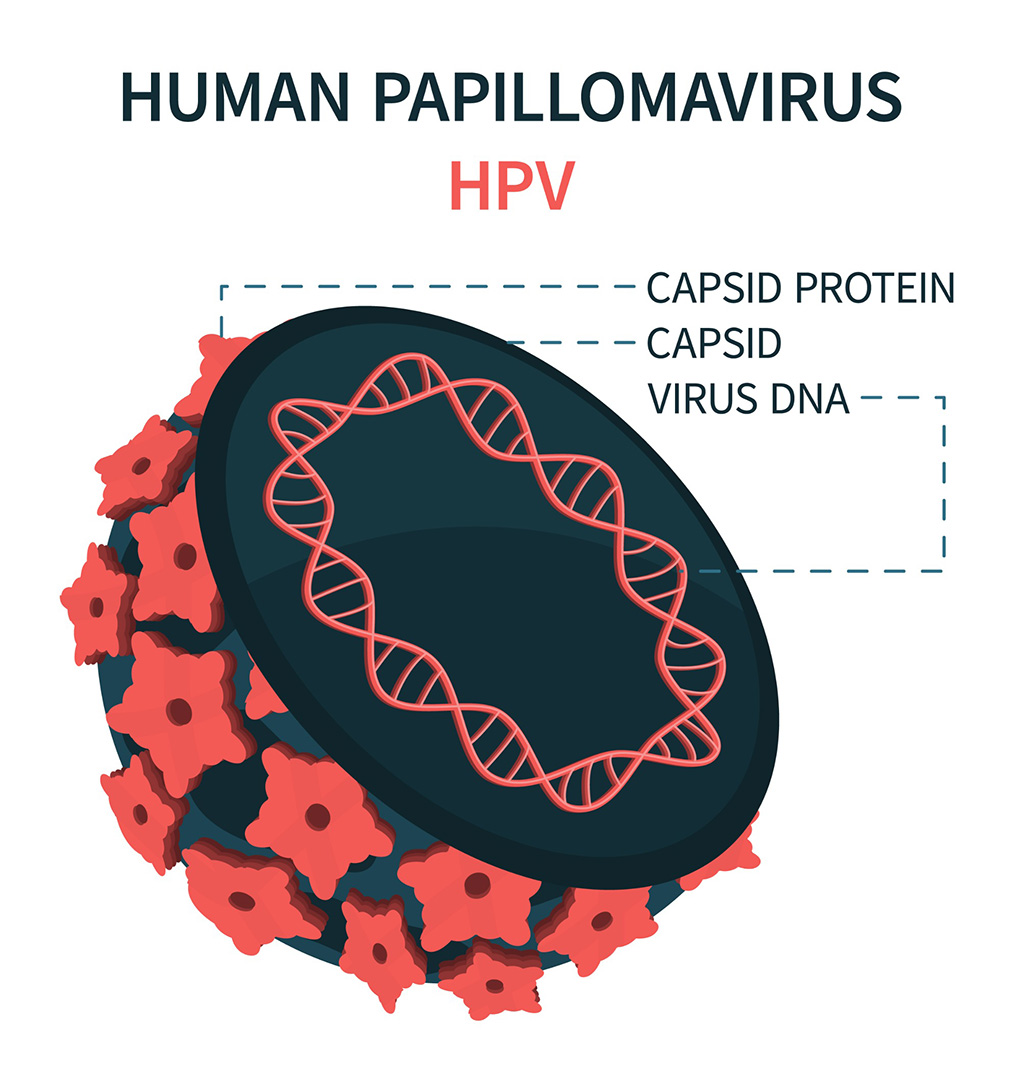
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more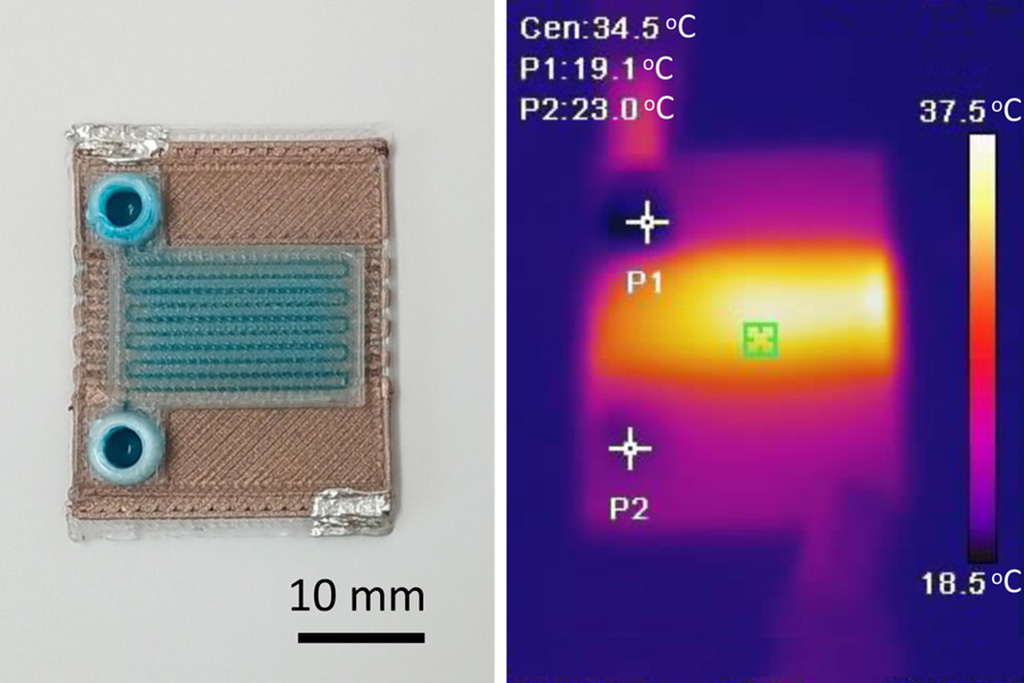
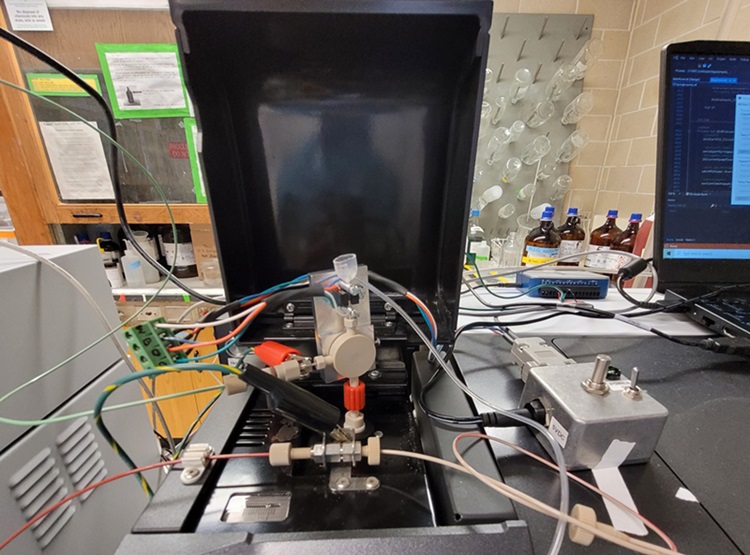
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel
Danaher and Johns Hopkins University Collaborate to Improve Neurological Diagnosis
Unlike severe traumatic brain injury (TBI), mild TBI often does not show clear correlations with abnormalities detected through head computed tomography (CT) scans. Consequently, there is a pressing need... Read more
Beckman Coulter and MeMed Expand Host Immune Response Diagnostics Partnership
Beckman Coulter Diagnostics (Brea, CA, USA) and MeMed BV (Haifa, Israel) have expanded their host immune response diagnostics partnership. Beckman Coulter is now an authorized distributor of the MeMed... Read more_1.jpg)











_1.jpg)
.jpg)
