Diagnostic Criteria for Multicentric Castleman Disease Published
|
By LabMedica International staff writers Posted on 28 Feb 2017 |
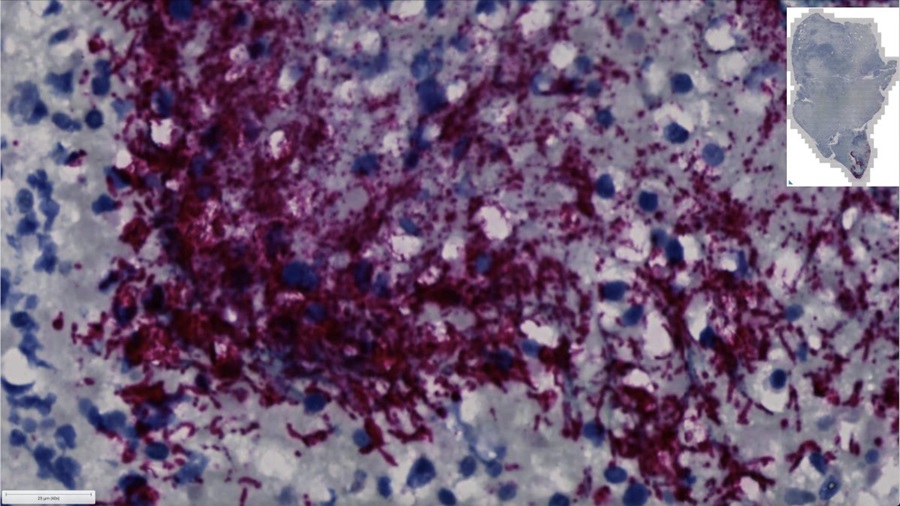
Image: A photomicrograph of lymph node tissue from a person with, idiopathic multicentric Castleman disease. Image shows increased number of blood vessels and smaller germinal centers where immune cells mature in the lymph node, which are two of the pathology features needed to make the diagnosis (Photo courtesy of Dr. David Fajgenbaum, University of Pennsylvania).
An international panel of experts in pediatric and adult hematopathology, hematology/oncology, rheumatology, immunology, and infectious diseases has established the first set of diagnostic criteria for idiopathic multicentric Castleman disease (iMCD).
Multicentric Castleman disease involves hyperactivation of the immune system, excessive release of proinflammatory cytokines, proliferation of immune cells (B-cells and T-cells), and multiple organ system dysfunction. Approximately 1,200 patients are diagnosed with iMCD each year in the United States. The disorder can occur in patients of any age, and about 35% of iMCD patients die within five years of diagnosis; 60% die within 10 years. In 2014, siltuximab, an anti-IL6 monoclonal antibody used to treat cancer, became the first [U.S.] Food and Drug Administration-approved iMCD therapy based on results from an international, randomized controlled trial in which 34% of patients had a complete or partial response to the drug compared to 0% on placebo.
Castleman disease must be distinguished from other disorders that can demonstrate "Castleman-like" lymph node features, including reactive lymph node hyperplasia, autoimmune disorders, and malignancies. Accurate diagnosis is challenging, as no standard diagnostic criteria or diagnostic biomarkers currently exist, and there is significant overlap with malignant, autoimmune, and infectious disorders. To correct the lack of diagnostic criteria, an international working group comprising 34 pediatric and adult pathology and clinical experts in iMCD and related disorders from eight countries, including two physicians that are also iMCD patients, was convened to establish iMCD diagnostic criteria. The working group reviewed data from 244 cases, met twice, and refined criteria over 15 months (June 2015 - September 2016).
The working group decided that for a diagnosis of iMCD to be made, two major criteria and at least two of 11 minor criteria are met, including at least one laboratory abnormality, such as anemia or elevated C-reactive protein in the blood. Additionally, several diseases with similar clinical presentation to iMCD must be excluded, such as another sub-type of CD called HHV-8-associated multicentric CD.
"Previously, patients had to hope their doctors were familiar with the Castleman disease medical literature in order for them to even consider an iMCD diagnosis," said first author David Fajgenbaum, assistant professor of medicine at the University of Pennsylvania. "Then, for the doctors considering the diagnosis, actually diagnosing it was very difficult. Now, with these criteria, doctors will know exactly what to look for and what to check off to feel confident about a diagnosis. The new criteria will accelerate time to diagnosis and, more importantly, administration of life-saving treatments for iMCD patients."
"I feel so pleased and optimistic that we are finally turning the tide against this disease," said Dr. Fajgenbaum. "I have heard of too many patients diagnosed with the disease only after they died and underwent an autopsy, and hopefully this will help doctors to diagnose it before it is too late."
Details of the diagnostic criteria were published in the January 13, 2017, online edition of the journal Blood.
Multicentric Castleman disease involves hyperactivation of the immune system, excessive release of proinflammatory cytokines, proliferation of immune cells (B-cells and T-cells), and multiple organ system dysfunction. Approximately 1,200 patients are diagnosed with iMCD each year in the United States. The disorder can occur in patients of any age, and about 35% of iMCD patients die within five years of diagnosis; 60% die within 10 years. In 2014, siltuximab, an anti-IL6 monoclonal antibody used to treat cancer, became the first [U.S.] Food and Drug Administration-approved iMCD therapy based on results from an international, randomized controlled trial in which 34% of patients had a complete or partial response to the drug compared to 0% on placebo.
Castleman disease must be distinguished from other disorders that can demonstrate "Castleman-like" lymph node features, including reactive lymph node hyperplasia, autoimmune disorders, and malignancies. Accurate diagnosis is challenging, as no standard diagnostic criteria or diagnostic biomarkers currently exist, and there is significant overlap with malignant, autoimmune, and infectious disorders. To correct the lack of diagnostic criteria, an international working group comprising 34 pediatric and adult pathology and clinical experts in iMCD and related disorders from eight countries, including two physicians that are also iMCD patients, was convened to establish iMCD diagnostic criteria. The working group reviewed data from 244 cases, met twice, and refined criteria over 15 months (June 2015 - September 2016).
The working group decided that for a diagnosis of iMCD to be made, two major criteria and at least two of 11 minor criteria are met, including at least one laboratory abnormality, such as anemia or elevated C-reactive protein in the blood. Additionally, several diseases with similar clinical presentation to iMCD must be excluded, such as another sub-type of CD called HHV-8-associated multicentric CD.
"Previously, patients had to hope their doctors were familiar with the Castleman disease medical literature in order for them to even consider an iMCD diagnosis," said first author David Fajgenbaum, assistant professor of medicine at the University of Pennsylvania. "Then, for the doctors considering the diagnosis, actually diagnosing it was very difficult. Now, with these criteria, doctors will know exactly what to look for and what to check off to feel confident about a diagnosis. The new criteria will accelerate time to diagnosis and, more importantly, administration of life-saving treatments for iMCD patients."
"I feel so pleased and optimistic that we are finally turning the tide against this disease," said Dr. Fajgenbaum. "I have heard of too many patients diagnosed with the disease only after they died and underwent an autopsy, and hopefully this will help doctors to diagnose it before it is too late."
Details of the diagnostic criteria were published in the January 13, 2017, online edition of the journal Blood.
Latest Pathology News
- Use of DICOM Images for Pathology Diagnostics Marks Significant Step towards Standardization
- First of Its Kind Universal Tool to Revolutionize Sample Collection for Diagnostic Tests
- AI-Powered Digital Imaging System to Revolutionize Cancer Diagnosis
- New Mycobacterium Tuberculosis Panel to Support Real-Time Surveillance and Combat Antimicrobial Resistance
- New Method Offers Sustainable Approach to Universal Metabolic Cancer Diagnosis
- Spatial Tissue Analysis Identifies Patterns Associated With Ovarian Cancer Relapse
- Unique Hand-Warming Technology Supports High-Quality Fingertip Blood Sample Collection
- Image-Based AI Shows Promise for Parasite Detection in Digitized Stool Samples
- Deep Learning Powered AI Algorithms Improve Skin Cancer Diagnostic Accuracy
- Microfluidic Device for Cancer Detection Precisely Separates Tumor Entities
- Virtual Skin Biopsy Determines Presence of Cancerous Cells
- AI Detects Viable Tumor Cells for Accurate Bone Cancer Prognoses Post Chemotherapy
- First Ever Technique Identifies Single Cancer Cells in Blood for Targeted Treatments
- Innovative Blood Collection Device Overcomes Common Obstacles Related to Phlebotomy
- Intra-Operative POC Device Distinguishes Between Benign and Malignant Ovarian Cysts within 15 Minutes
- Simple Skin Biopsy Test Detects Parkinson’s and Related Neurodegenerative Diseases
Channels
Clinical Chemistry
view channel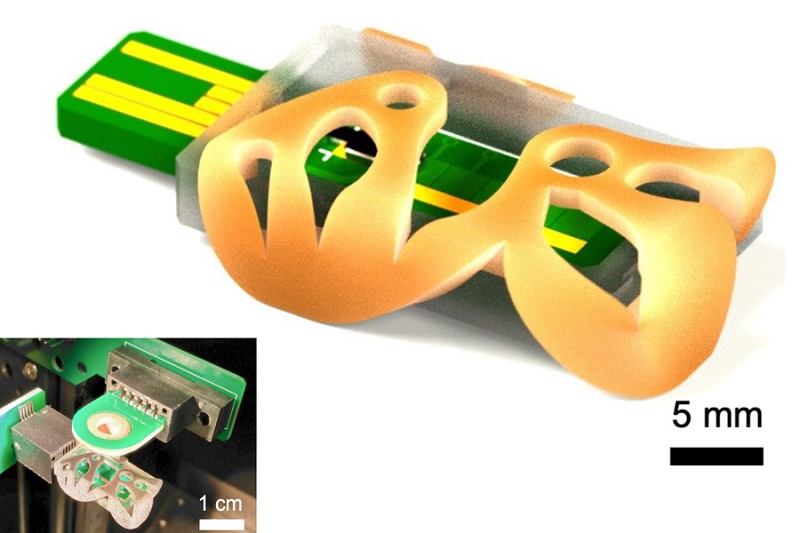
3D Printed Point-Of-Care Mass Spectrometer Outperforms State-Of-The-Art Models
Mass spectrometry is a precise technique for identifying the chemical components of a sample and has significant potential for monitoring chronic illness health states, such as measuring hormone levels... Read more.jpg)
POC Biomedical Test Spins Water Droplet Using Sound Waves for Cancer Detection
Exosomes, tiny cellular bioparticles carrying a specific set of proteins, lipids, and genetic materials, play a crucial role in cell communication and hold promise for non-invasive diagnostics.... Read more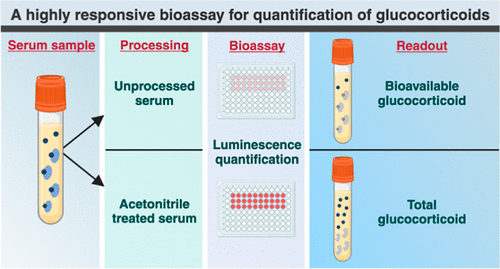
Highly Reliable Cell-Based Assay Enables Accurate Diagnosis of Endocrine Diseases
The conventional methods for measuring free cortisol, the body's stress hormone, from blood or saliva are quite demanding and require sample processing. The most common method, therefore, involves collecting... Read moreMolecular Diagnostics
view channel
New Genetic Testing Procedure Combined With Ultrasound Detects High Cardiovascular Risk
A key interest area in cardiovascular research today is the impact of clonal hematopoiesis on cardiovascular diseases. Clonal hematopoiesis results from mutations in hematopoietic stem cells and may lead... Read more
Blood Samples Enhance B-Cell Lymphoma Diagnostics and Prognosis
B-cell lymphoma is the predominant form of cancer affecting the lymphatic system, with about 30% of patients with aggressive forms of this disease experiencing relapse. Currently, the disease’s risk assessment... Read moreHematology
view channel
Next Generation Instrument Screens for Hemoglobin Disorders in Newborns
Hemoglobinopathies, the most widespread inherited conditions globally, affect about 7% of the population as carriers, with 2.7% of newborns being born with these conditions. The spectrum of clinical manifestations... Read more
First 4-in-1 Nucleic Acid Test for Arbovirus Screening to Reduce Risk of Transfusion-Transmitted Infections
Arboviruses represent an emerging global health threat, exacerbated by climate change and increased international travel that is facilitating their spread across new regions. Chikungunya, dengue, West... Read more
POC Finger-Prick Blood Test Determines Risk of Neutropenic Sepsis in Patients Undergoing Chemotherapy
Neutropenia, a decrease in neutrophils (a type of white blood cell crucial for fighting infections), is a frequent side effect of certain cancer treatments. This condition elevates the risk of infections,... Read more
First Affordable and Rapid Test for Beta Thalassemia Demonstrates 99% Diagnostic Accuracy
Hemoglobin disorders rank as some of the most prevalent monogenic diseases globally. Among various hemoglobin disorders, beta thalassemia, a hereditary blood disorder, affects about 1.5% of the world's... Read moreImmunology
view channel
Diagnostic Blood Test for Cellular Rejection after Organ Transplant Could Replace Surgical Biopsies
Transplanted organs constantly face the risk of being rejected by the recipient's immune system which differentiates self from non-self using T cells and B cells. T cells are commonly associated with acute... Read more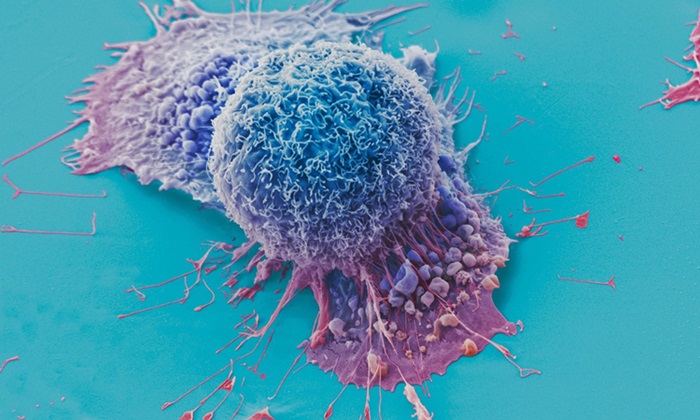
AI Tool Precisely Matches Cancer Drugs to Patients Using Information from Each Tumor Cell
Current strategies for matching cancer patients with specific treatments often depend on bulk sequencing of tumor DNA and RNA, which provides an average profile from all cells within a tumor sample.... Read more
Genetic Testing Combined With Personalized Drug Screening On Tumor Samples to Revolutionize Cancer Treatment
Cancer treatment typically adheres to a standard of care—established, statistically validated regimens that are effective for the majority of patients. However, the disease’s inherent variability means... Read moreMicrobiology
view channel
Clinical Decision Support Software a Game-Changer in Antimicrobial Resistance Battle
Antimicrobial resistance (AMR) is a serious global public health concern that claims millions of lives every year. It primarily results from the inappropriate and excessive use of antibiotics, which reduces... Read more
New CE-Marked Hepatitis Assays to Help Diagnose Infections Earlier
According to the World Health Organization (WHO), an estimated 354 million individuals globally are afflicted with chronic hepatitis B or C. These viruses are the leading causes of liver cirrhosis, liver... Read more
1 Hour, Direct-From-Blood Multiplex PCR Test Identifies 95% of Sepsis-Causing Pathogens
Sepsis contributes to one in every three hospital deaths in the US, and globally, septic shock carries a mortality rate of 30-40%. Diagnosing sepsis early is challenging due to its non-specific symptoms... Read moreTechnology
view channel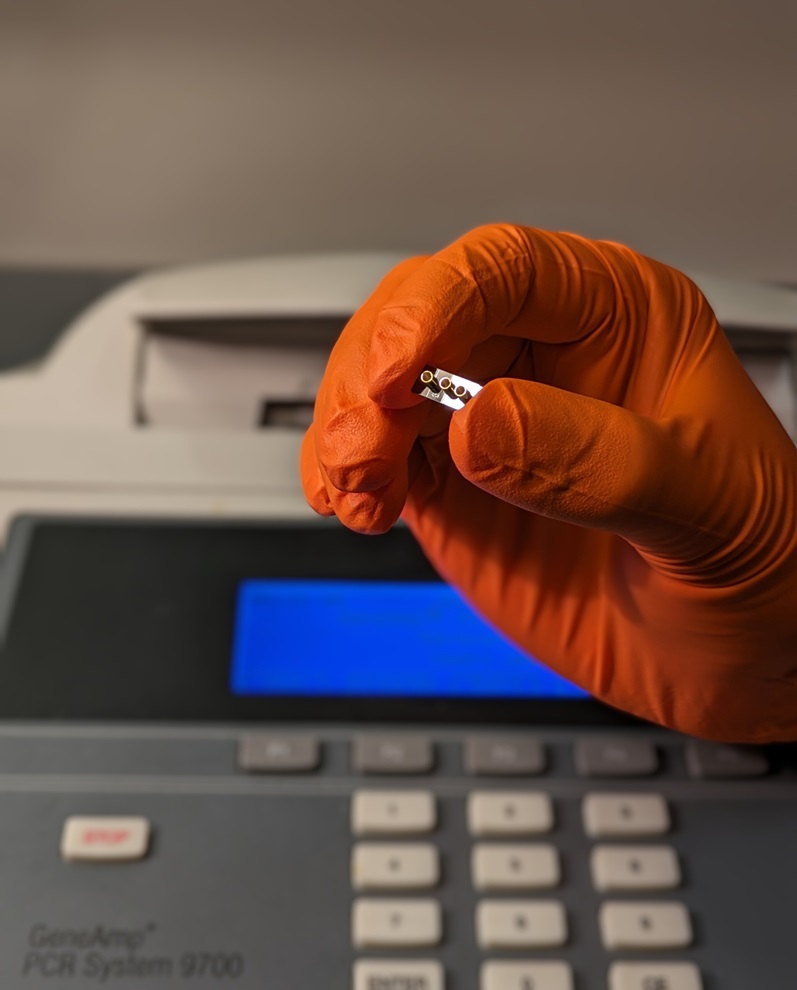
New Diagnostic System Achieves PCR Testing Accuracy
While PCR tests are the gold standard of accuracy for virology testing, they come with limitations such as complexity, the need for skilled lab operators, and longer result times. They also require complex... Read more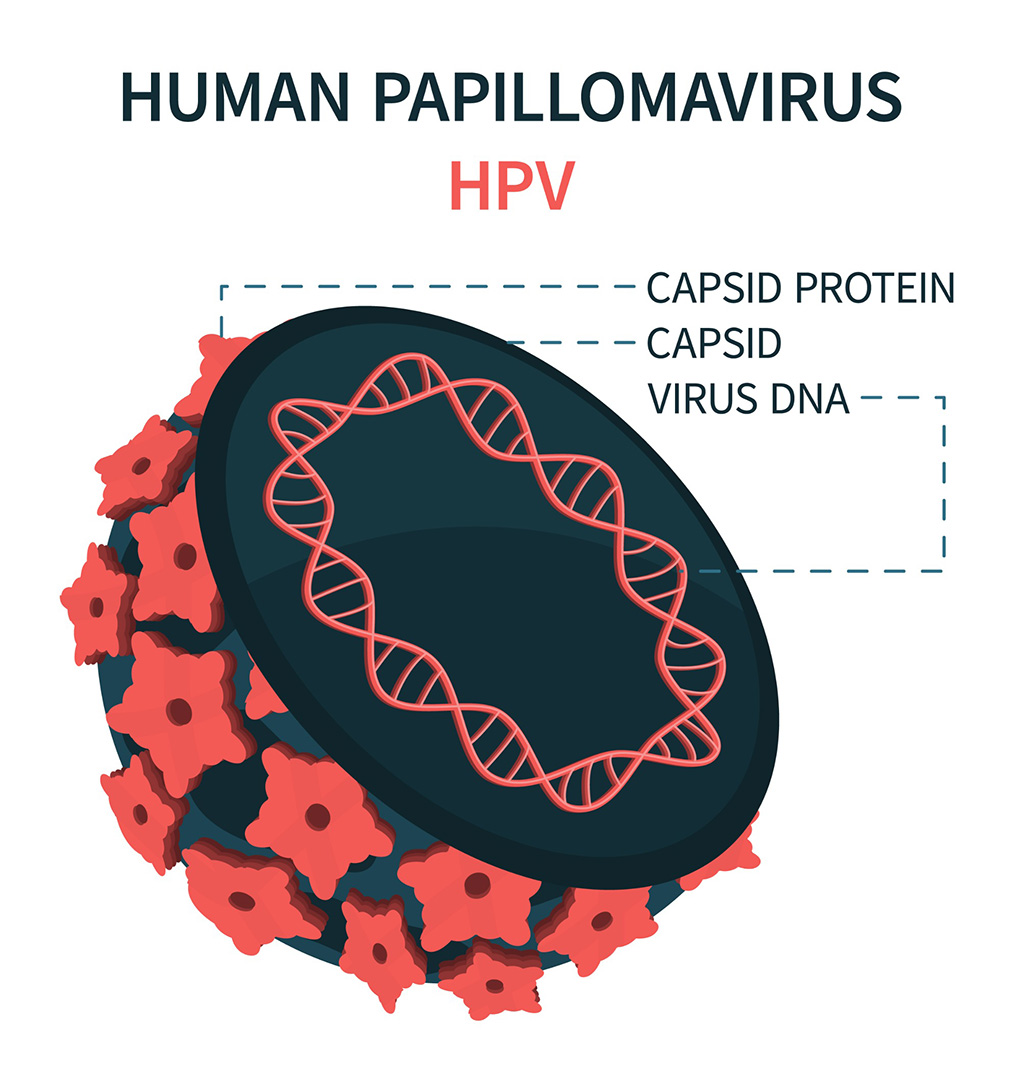
DNA Biosensor Enables Early Diagnosis of Cervical Cancer
Molybdenum disulfide (MoS2), recognized for its potential to form two-dimensional nanosheets like graphene, is a material that's increasingly catching the eye of the scientific community.... Read more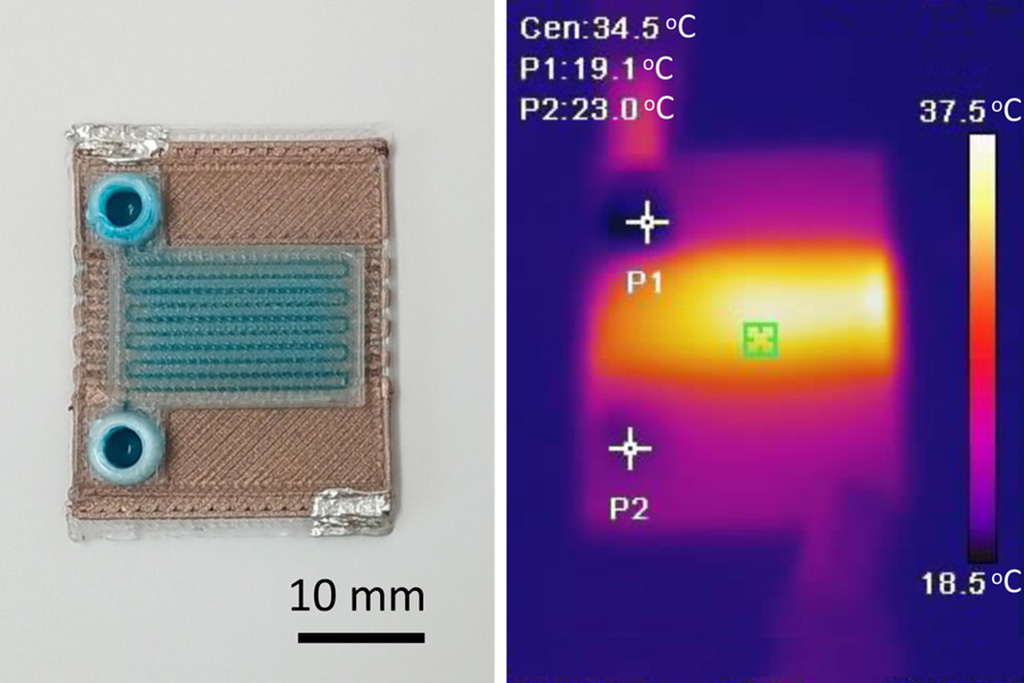
Self-Heating Microfluidic Devices Can Detect Diseases in Tiny Blood or Fluid Samples
Microfluidics, which are miniature devices that control the flow of liquids and facilitate chemical reactions, play a key role in disease detection from small samples of blood or other fluids.... Read more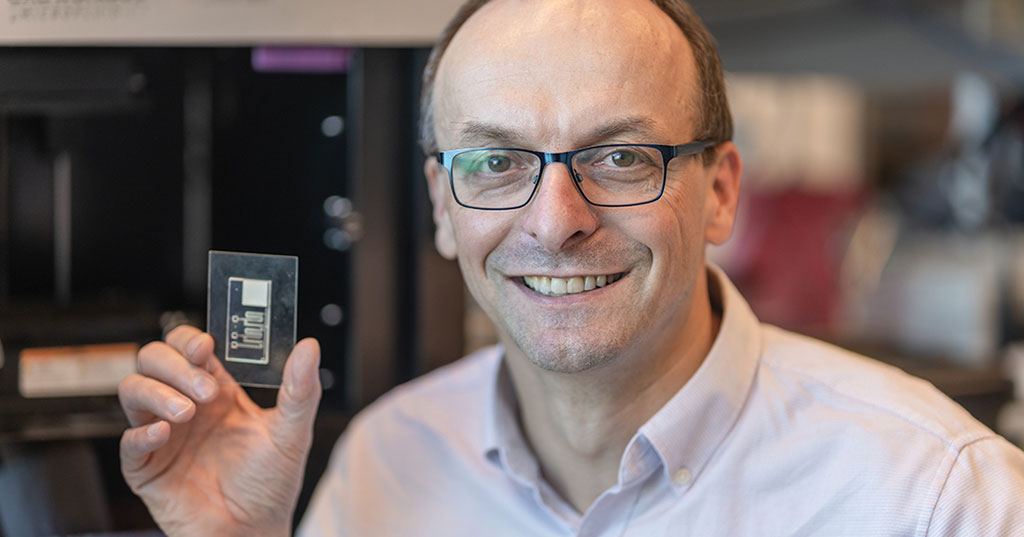
Breakthrough in Diagnostic Technology Could Make On-The-Spot Testing Widely Accessible
Home testing gained significant importance during the COVID-19 pandemic, yet the availability of rapid tests is limited, and most of them can only drive one liquid across the strip, leading to continued... Read moreIndustry
view channel_1.jpg)
Thermo Fisher and Bio-Techne Enter Into Strategic Distribution Agreement for Europe
Thermo Fisher Scientific (Waltham, MA USA) has entered into a strategic distribution agreement with Bio-Techne Corporation (Minneapolis, MN, USA), resulting in a significant collaboration between two industry... Read more
ECCMID Congress Name Changes to ESCMID Global
Over the last few years, the European Society of Clinical Microbiology and Infectious Diseases (ESCMID, Basel, Switzerland) has evolved remarkably. The society is now stronger and broader than ever before... Read more