Electronic Nose Technology May Facilitate Accurate Diagnosis of Sarcoidosis
Posted on 12 Apr 2022
Sarcoidosis is a granulomatous inflammatory disease without a known cause that can affect roughly any organ. The lungs are involved in the vast majority of patients (89% to 99%). Diagnosis can be challenging because no standardized diagnostic procedure exists. The three major criteria for diagnosis are compatible clinical features, pathology tissue assessment, and exclusion of other granulomatous diagnoses.
Breath biomarkers are increasingly studied in respiratory diseases, as exhaled volatile organic compounds (VOCs) reflect pathophysiological processes in the human body. Techniques such as gas chromatography and mass spectrometry can be used to identify individual VOCs, but are time-consuming and complex. Analysis of a profile of VOCs (a “breathprint”) using electronic nose (eNose) technology will be of added value in clinical practice.
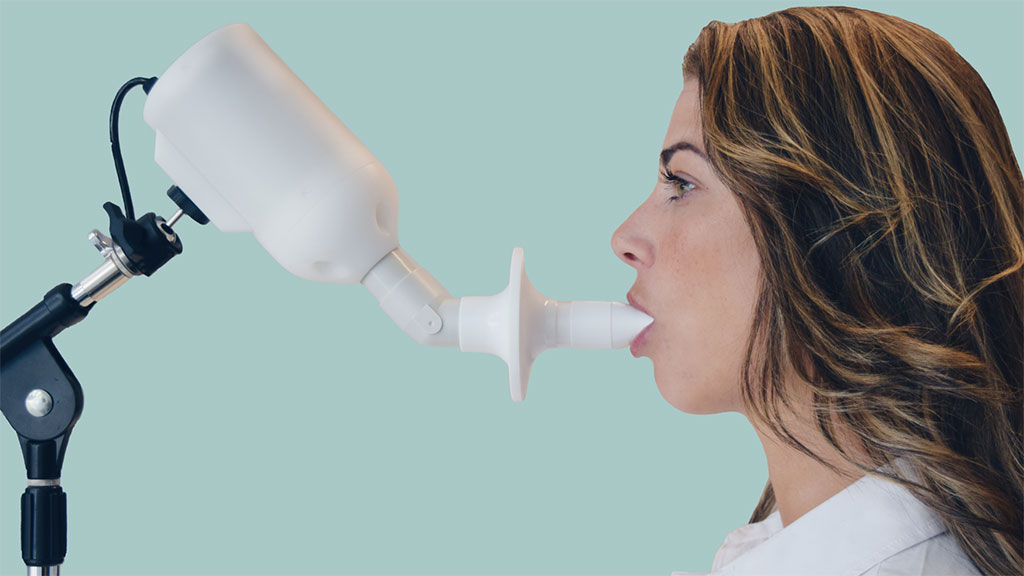
Respiratory Medicine Specialists at the Erasmus Medical Center (Rotterdam, The Netherlands) included in cross-sectional study 252 patients with sarcoidosis (mean age, 53.1 years; 53.2% men), 317 with interstitial lung disease (ILD, mean age, 70 years; 61.5% men), and 48 healthy control subjects (mean age, 36.5 years; 31.3% men). The SpiroNose (Breathomix, Leiden, The Netherlands) was used for exhaled breath analysis. Participants were instructed to perform five tidal breaths, followed by an inhalation to total lung capacity, a 5 second breath hold, and a slow expiration. To explore if breathprints correlate with disease activity, the soluble interleukin-2 receptor (sIL-2R) level was used as a marker for activity. In the laboratory, an sIL-2R value ≤ 550 U/mL was considered normal.
The team reported that eNose distinguished sarcoidosis from control subjects with an area under the curve (AUC) of 1.00 and pulmonary sarcoidosis from other ILD (AUC, 0.87) and hypersensitivity pneumonitis (AUC, 0.88). Exhaled breath of sarcoidosis patients with and without pulmonary involvement, pulmonary fibrosis, multiple organ involvement, pathology-supported diagnosis, and immunosuppressive treatment revealed no distinctive differences. Breath profiles differed between patients with a slightly and highly elevated soluble IL-2 receptor level (median cutoff, 772.0 U/mL; AUC, 0.78).
Iris G. van der Sar, MD, the lead author of the study, said, “Currently, diagnosis of sarcoidosis is challenging due to great differences in clinical presentation often requiring invasive diagnostic procedures such as biopsies. The accuracy of eNose technology is much higher than for other diagnostic tests used in clinical practice for sarcoidosis patients. Building a diagnostic algorithm will allow doctors to use the eNose technology in clinical decision-making in the future.”
The authors concluded that their study showed a reliable and accurate differentiation of patients with sarcoidosis from patients with ILD and healthy control subjects, based on eNose data. The results confirm the potential of eNose technology as a noninvasive diagnostic tool to obtain an early, accurate sarcoidosis diagnosis and reduce the number of invasive diagnostic procedures in the diagnostic trajectory. The study was published on March 1, 2022 in the journal Chest.
Related Links:
Erasmus Medical Center
Breathomix