Topical Fluorescent Imaging Technique Detects Basal Cell Carcinoma
Posted on 27 Aug 2025
Basal cell carcinoma is the most common skin cancer, and while early treatment often leads to excellent outcomes, diagnosis typically requires biopsy. This invasive procedure can be painful, leave scars, and delay treatment due to the time needed for histopathologic confirmation. To address these challenges, researchers have now developed a novel topical fluorescent imaging technique that can detect basal cell carcinoma through intact skin within minutes.
The new approach developed by researchers at Memorial Sloan Kettering Cancer Center (MSK, New York, NY, USA) relies on a topical fluorescent molecular contrast agent called PARPi-FL. The method uses fluorescent confocal microscopy to enhance cancer detection, offering a potential noninvasive alternative to standard biopsy. Unlike conventional tools, PARPi-FL can be applied topically, is non-toxic to the skin, and does not cause systemic side effects, making it safe for use in clinical settings.
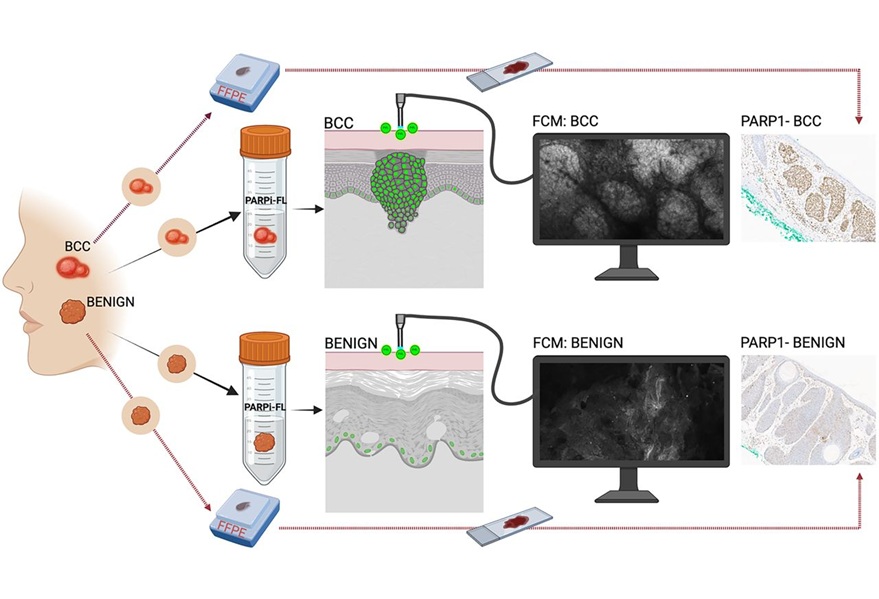
To evaluate this innovation, researchers tested PARPi-FL on ex vivo human tissues, including specimens from plastic surgery, Mohs surgery, and fresh excisions of both benign and cancerous tissues. They also explored topical application methods using gauze and assessed real-time in vivo imaging in tumor-bearing mice. Safety was further confirmed through preclinical toxicology studies, showing that the agent is well-tolerated.
The findings, published in The Journal of Nuclear Medicine, show that applying a minimal topical dose of PARPi-FL for two to five minutes produced strong fluorescent signals in basal cell carcinoma lesions while generating significantly weaker signals in benign tissues. These findings highlight the diagnostic accuracy of the technique, demonstrating its ability to distinguish malignant from benign lesions. The data confirmed that the approach could reliably detect tumors without harming surrounding skin.
Going forward, integrating PARPi-FL with in vivo imaging devices could improve diagnostic precision and reduce unnecessary biopsies of benign lesions. The method also holds promise for timely, noninvasive treatments at the bedside. Importantly, since PARP1 is also overexpressed in melanoma, the technology may be extended to detect and differentiate other skin cancers, expanding its potential clinical applications.
Related Links:
MSK














