New AI Protocol Instantaneously Detects Cancer Genomic Biomarkers Directly from Tumor Biopsy Slides
Posted on 05 Aug 2024
The late 90s marked the beginning of the era of precision oncology, yet recent studies in the U.S. indicate that most cancer patients are not receiving FDA-approved precision therapies. Factors such as high costs, extensive tissue requirements, and lengthy processing times have hampered the broader adoption of precision oncology, often leading to treatments that are not only suboptimal but potentially harmful. A significant barrier is the lack of testing; many cancer patients endure critical delays waiting for standard genomic tests following an initial tumor diagnosis, which can be life-threatening. Now, a groundbreaking advancement has been made with the development of a new generation of artificial intelligence (AI) tools that enable the rapid and cost-effective detection of clinically actionable genomic alterations directly from tumor biopsy slides. This innovation could cut weeks and save thousands of dollars in clinical oncology treatment workflows for diseases like breast and ovarian cancers.
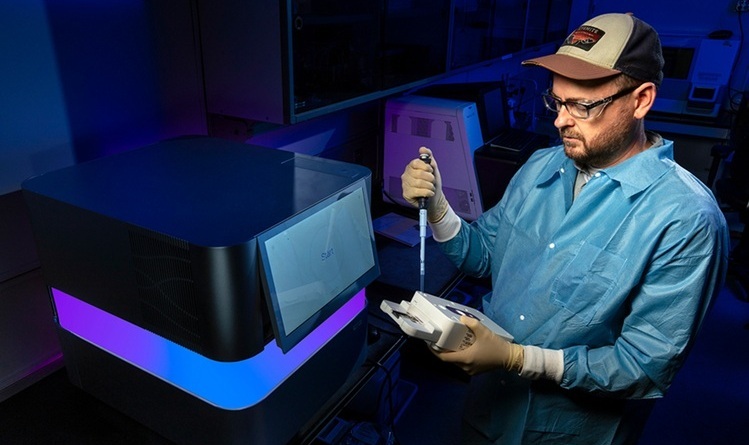
The new AI protocol, termed DeepHRD, was developed by researchers at the University of California San Diego (La Jolla, CA, USA). It marks a significant leap forward in eliminating the delays and health disparities undermining the potential of precision medicine for cancer patients. The tool leverages minimal patient information available early in the diagnostic process. Almost every cancer patient undergoes a tumor biopsy, which is traditionally processed and reviewed under a light microscope—a method established in the late 19th century and still foundational in early oncology workflows. The DeepHRD AI protocol can be applied directly to standard tissue slides for instant and accurate identification of genomic cancer biomarkers, as detailed in research published in the Journal of Clinical Oncology.
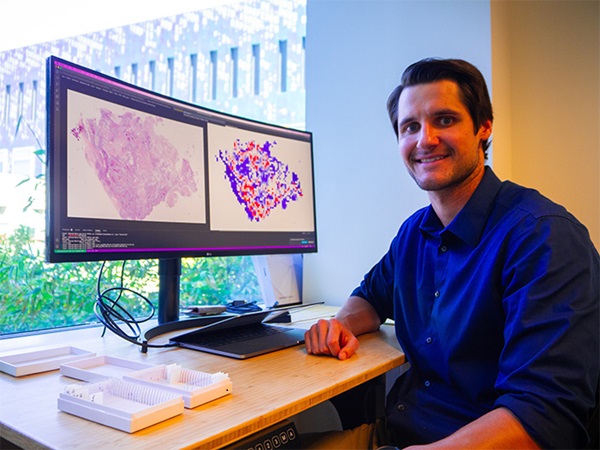
The AI specifically identifies biomarkers for homologous recombination deficiency (HRD), a critical DNA damage repair mechanism loss. Ovarian and breast cancer patients with HRD typically respond well to platinum and PARP (poly-ADP ribose polymerase) inhibitor therapies. This AI model can dramatically expedite treatment decisions immediately following the initial tissue diagnosis, offering a significant time advantage. Unlike traditional genomic testing, which has a failure rate of 20 to 30 percent necessitating re-tests or further invasive biopsies, this AI tool exhibits a virtually zero failure rate.
This technology is poised to democratize access to critical genomic biomarker detection for precision therapy, thus enabling equitable treatment options for advanced cancer patients globally. It holds particular promise for bridging significant gaps in precision medicine, especially in under-resourced or remote areas where such testing is less common. The researchers are now working to rapidly transition this AI platform to clinical settings, aiming to make precision therapy a reality for more patients by providing faster access to appropriate treatments. They anticipate that this technology could eventually apply to a wide range of genomic biomarkers and numerous cancer types.