Prognostic Value of Specific Biomarker in Prostate Cancer Authenticated
By LabMedica International staff writers
Posted on 20 Aug 2019
Prostate cancer (PC) is the most commonly diagnosed cancer in Canadian men. In men with high-risk PC, progression of the disease will lead to biochemical recurrence (BCR), distant metastases, and disease-specific mortality.Posted on 20 Aug 2019
The extensively studied nuclear factor kappa B (NF-κB) pathway is involved in the regulation of inflammation and the immune response, and more recently demonstrated its importance in cancer development. The activation of the NF-κB signaling pathways can result in the progression of several types of cancer, including PC.
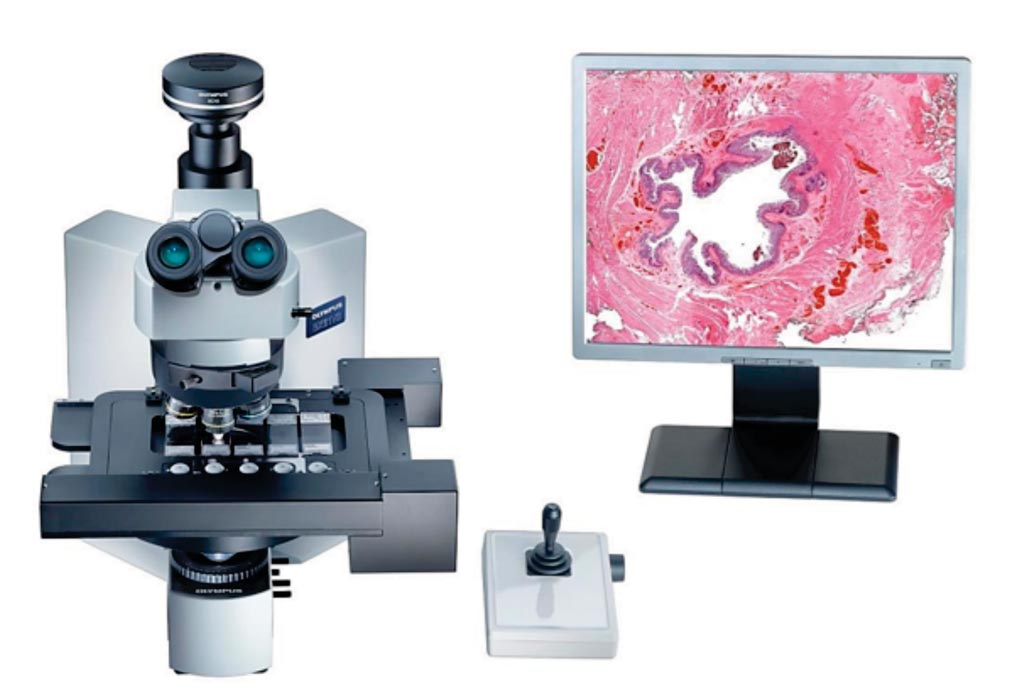
Image: The VS110 combines microscopy seamlessly with imaging to create a virtual slide that is an exact copy of the real specimen (Photo courtesy of Olympus).
A large team of scientists at the Centre hospitalier de l’Université de Montréal (Montreal, QC, Canada) and their associates accessed two different multi-center tissue microarrays (TMAs) representing cohorts of patients (Test-TMA and Validation-TMA series) of the Canadian Prostate Cancer Biomarker Network (CPCBN) to validate the association between p65 nuclear frequency and PC outcomes. Immunohistochemical staining of p65 was performed on the Test-TMA and Validation-TMA series, which include PC tissues from patients treated by first-line radical prostatectomy (n = 250 and n = 1,262, respectively).
For each patient, 0.6-mm cores (3–4 of tumor tissue and 1–2 of benign adjacent tissue) were punctured from formalin-fixed paraffin-embedded blocks and transferred to receiver blocks. Four-micrometer-thick sections of each TMA block were subjected to antigen retrieval in Cell Conditioning 1 for 90 minutes and then stained using the BenchMark XT autostainer. All sections were scanned using a VS-110 microscope with a 20× 0.75 NA objective and a resolution of 0.3225 μm. Two independent observers evaluated the p65 nuclear frequency in digital images of cancer tissue and benign adjacent gland tissue.
Multivariate analysis of the Validation-TMA cohort showed that p65 nuclear frequency in cancer cells was an independent predictor of BCR using continuous (hazard ratio [HR] 1.02) and dichotomized data (HR 1.33). The team used a cutoff of 3%, and found that this biomarker was also associated with the development of bone metastases (HR 1.82) and PC-specific mortality (HR 2.63), independent of clinical parameters. BCR-free survival, bone-metastasis-free survival, and PC-specific survival were shorter for patients with higher p65 nuclear frequency.
The authors concluded that they had demonstrated the prognostic significance of nuclear p65 in two independent PC TMA cohorts that included primary tumor tissues of patients from multiple institutions. The implementation of this biomarker in the clinical workflow would allow genitourinary pathologists and clinicians to improve the identification of patients with high-risk PC. The study was published on July 2, 2019, in the journal PLOS Medicine.
Related Links:
Centre hospitalier de l’Université de Montréal














