Blood Test Predicts Kidney Transplant Rejection
By LabMedica International staff writers
Posted on 12 Mar 2019
A renal transplant offers the best treatment for patients whose kidneys have failed, with around 3,000 carried out annually in the UK. Acute rejection occurs when the body's immune system begins to attack the donated organ.Posted on 12 Mar 2019
This rejection is a common complication in the first year after the transplant, affecting around two in 10 patients. It can affect the lifespan of the transplanted organ. Currently, acute rejection can only be confirmed by taking a biopsy of the transplanted organ. While acute rejection can be treated, this can only be done when the organ is already affected and damage has already occurred.
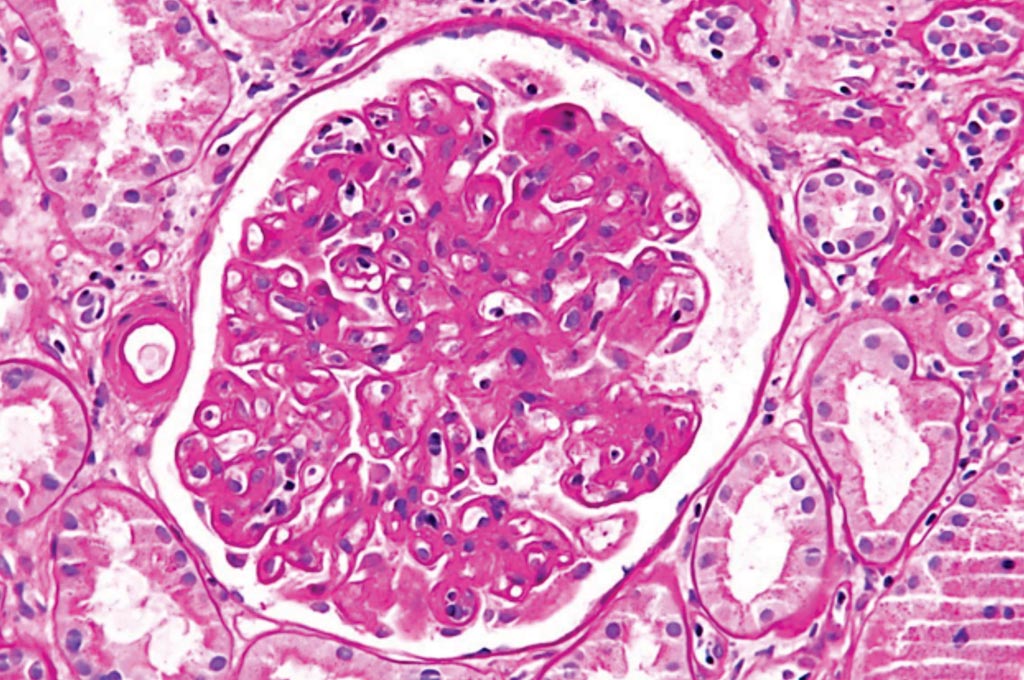
Image: A photomicrograph of a glomerulus with changes characteristic of a transplant glomerulopathy. Transplant glomerulopathy is considered a form of chronic antibody-mediated rejection (Photo courtesy of Nephron).
Scientists at the Guy's and St Thomas' NSH Foundation Trust (London, UK) and their colleagues collected blood samples serially from 455 consecutive kidney transplant recipients (KTRs), transplanted at a single regional transplant center. Samples were collected at 26 time-points during clinic visits over the first post-transplant year. A total of 1,464 samples from 248 patients were used in the study, including 66 patients with an episode of rejection.
The team examined the quantitative reverse transcription polymerase chain reaction (RT-qPCR) expression of 22 literature-based genes in peripheral blood samples from 248 patients. To select genes, they used penalized logistic regression based on 27 stable patients and 27 rejectors with biopsy-proven T-cell-mediated rejection, fulfilling strict inclusion/exclusion criteria. They validated this signature in an independent group of stable patients and patients with concomitant T-cell and antibody-mediated-rejection; patients from an independent study; and cross-sectional pre-biopsy samples from non-rejectors, and longitudinal follow-up samples covering the first post-transplant year from rejectors, non-rejectors and stable patients.
Using these samples and analyzing the data over time, they developed a signature combination of seven genes that differentiated patients who developed rejection from those who did not. A parsimonious acute T-cell mediated rejection (TCMR)-signature (IFNG, IP-10, ITGA4, MARCH8, RORc, SEMA7A, and WDR40A) showed cross-validated area-under-ROC curve 0.84. The team also identified a six-gene signature for a less common form of complication. BK-virus nephropathy can look clinically similar to acute rejection, but requires a very different therapy, reducing immunosuppression. Being able to distinguish between these complications would mean clinicians can ensure that patients receive the most appropriate treatment.
The authors concluded that molecular marker alterations in blood emerge well ahead of the time of clinically overt TCMR. Monitoring a TCMR-signature in peripheral blood could unravel T-cell-related pro-inflammatory activity and hidden immunological processes. This additional information could support clinical management decisions in cases of patients with stable but poor kidney function or with inconclusive biopsy results.
Paramit Chowdhury, MD, PhD, a consultant nephrologist and a senior author of the study, said, “This advance could make a huge difference to our ability to monitor kidney transplant patients and treat rejection earlier. It may also save some patients from an unnecessary biopsy. It is a first step in getting a better insight into the status of a patient's immune system, allowing better tailoring of the patient's anti-rejection treatment.” The study was published on March 1, 2019, in the journal EBioMedicine.
Related Links:
Guy's and St Thomas' NSH Foundation Trust