Risk for Colorectal Cancer Linked to Polyps and Adenomas
By LabMedica International staff writers
Posted on 25 Oct 2017
Most colorectal cancer develops from precursors known as polyps, the most common of which are conventional adenomas. Conventional adenomas often progress to colorectal cancer through an intermediate step called high-risk adenomas.Posted on 25 Oct 2017
Another type of polyp known as serrated polyps may proceed up to 15% of colorectal cancer. Serrated polyps may occur in up to 20% of all adults over 50 years of age, however, when it comes to progression to colorectal cancer, less is known about serrated polyps than conventional adenomas.
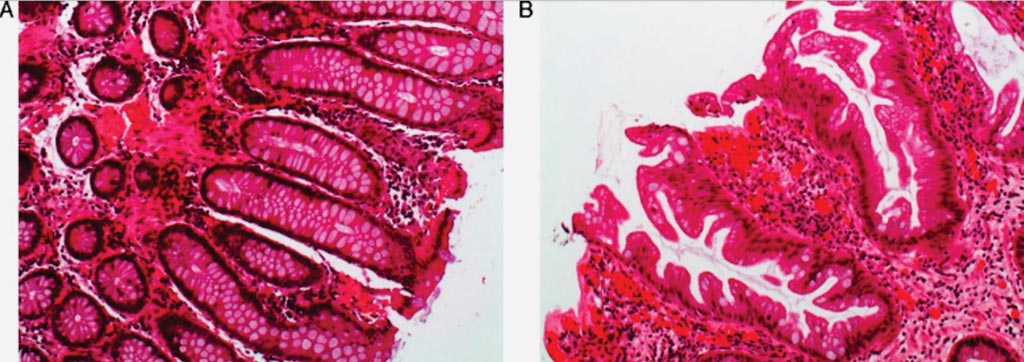
Image: The histologic appearance of serrated polyps: (A) normal colon mucosa; (B) sessile serrated adenoma with saw tooth appearance of the crypts in the longitudinal cut (Photo courtesy of Dr. Cuatrecasas).
Scientists at the Dartmouth-Hitchcock Medical Center (Lebanon, NH, USA) collected data from a population-based colonoscopy registry that has been collecting and analyzing data on colonoscopies across the state of New Hampshire since 2004, including rates of adenoma and serrated polyp detection. Patients completed a questionnaire to determine demographic characteristics, health history, and risk factors for colorectal cancer (CRC), and were followed from index colonoscopy through all subsequent surveillance colonoscopies. The analyses included 5,433 participants (median age 61 years; 49.7% male) with two colonoscopies (median time to surveillance, 4.9 years).
Each index risk group, were assessed for size and by histology. Two analyses were performed. The primary analysis compared 817 participants with high-risk adenoma (HRA) with or without synchronous serrated polyps (SP) and those 3,198 with no adenoma with or without synchronous serrated polyps at index colonoscopy. The secondary analysis included 1,418 participants with low risk adenoma (LRA) with and without synchronous serrated polyps and those 3,198 with no adenoma with and without serrated polyps at index colonoscopy.
The investigators found that HRA and synchronous large SP (odds ratio [OR] = 5.61), HRA with synchronous traditional serrated adenomas (STSA) (OR = 16.04), and HRA alone (OR = 3.86) at index colonoscopy significantly increased the risk of metachronous HRA compared to the reference group (no index adenomas or serrated polyps). Large index SPs alone (OR=14.34) or index STSA alone (OR = 9.70) significantly increased the risk of a large metachronous SP.
The authors concluded that in an analysis of data from a population-based colonoscopy registry, they found index large SP or index STSA with no index HRA increased risk of metachronous large SPs but not metachronous HRA. HRA and synchronous SPs at index colonoscopy significantly increased risk of metachronous HRA. Individuals with HRA and synchronous could therefore benefit from close surveillance.
Joseph C. Anderson, MD, the lead author of the study, said, “We found that while people with serrated polyps were at increased risk for future serrated polyps, they were not at risk for future high-risk adenomas. Not surprisingly, people with high-risk adenomas were at increased risk for high-risk adenomas. However, we made a novel observation that people with both serrated polyps and high-risk adenomas had a risk for future high-risk adenomas that was substantially higher than even people with high-risk adenomas alone.” The study was published on September 16, 2017, in the journal Gastroenterology.
Related Links:
Dartmouth-Hitchcock Medical Center