Bacterial Infection Associated with Sjögren’s Syndrome Risk
By LabMedica International staff writers
Posted on 27 Jun 2017
In a population-based case-control study, researchers have found a link between newly diagnosed Sjögren’s syndrome (SjS) and previous infection with nontuberculous mycobacteria (NTM). Although an increased risk of tuberculosis (TB) has previously been found in patients with SjS, in this study TB infection itself did not appear to be associated with an increased risk of developing SjS.Posted on 27 Jun 2017
Patients newly diagnosed with primary SjS (primary i.e. patients with no other rheumatic disease; specifically excluded were SjS patients with rheumatoid arthritis (RA) or systemic lupus erythematosus (lupus)) were around 11 times more likely to have had a prior infection with NTM than a matched group of controls. The magnitude of the association between NTM and SjS risk was greatest among those patients aged between 45-65 years. No association was found between SjS and a previous TB infection.
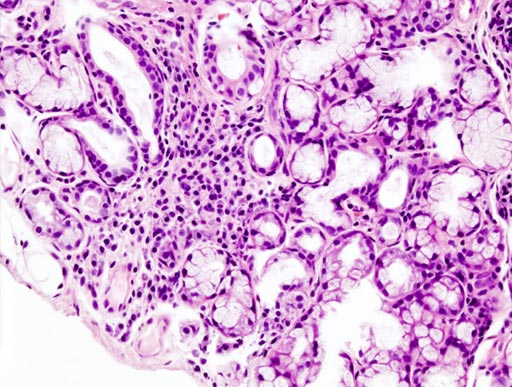
Image: A histopathologic image of focal lymphoid infiltration in the minor salivary gland associated with Sjögren syndrome (Photo courtesy of Wikimedia).
The diagnosis of NTM was established using ICD9-CM disease codes, as well as the prescription of NTM-related antibacterial medication. The association was quantified after adjusting for the Charlson comorbidity index (a standardized method for classifying comorbid conditions that increase the risk of 1-year mortality) and bronchiectasis (long-term condition that make lungs more vulnerable to infection).
“Although the exact disease mechanism behind SjS remains elusive, a variety of environmental, genetic, and hormonal factors have been linked with the development and different manifestations of this debilitating disease,” said lead author Dr. Hsin-Hua Chen from Taichung Veterans General Hospital (Taiwan, Province of China), “Identifying NTM as one of the triggers will hopefully provide a clue to the future development of a targeted therapy for these patients.”
“Because SjS is a disease of insidious onset, we can't exclude the possibility that it may have occurred before the NTM infection. In our study, of the 7 subjects with NTM infection later diagnosed with SjS, 3 of them were diagnosed within three months of NTM infection, indicating the potential coexistence of these two diseases. However, the other 4 subjects were diagnosed on average 2.9 years after NTM infection,” said Dr. Chen, “The significant association between NTM infection and newly diagnosed SjS demonstrated in our study certainly supports the need to screen for the presence of SjS in any patient previously infected with NTM to enable prompt diagnosis and treatment."
SjS is an immune mediated chronic inflammatory disease where the body’s immune system attacks glands that secrete fluid, such as the tear and saliva glands. Primary SjS occurs in people with no other rheumatic disease; secondary SjS occurs in people who have another rheumatic disease – about half of patients also RA or other connective tissue diseases, such as lupus. SjS can affect people of any age, but symptoms usually appear between the ages of 45 and 55. It affects 10 times as many women as men.
A EULAR initiative – “Don’t Delay, Connect Today” – unites people from patient organizations, scientific member societies, and health professional associations with the campaign goal of highlighting the importance of early diagnosis of RMDs and early access to treatment, in order to help prevent further damage and reduce the burden on individual life and on society as a whole.
Results from the study were presented by Chen H-H, Chao W-C, Liao T-L, et al, at the Annual European Congress of Rheumatology.
Related Links:
Taichung Veterans General Hospital