Blood Test Monitors Relapsed Serous Ovarian Cancer
By LabMedica International staff writers
Posted on 09 Feb 2017
The development of blood biomarkers that can be used for early detection of cancer or to measure tumor burden and response to treatment is a major goal of translational cancer studies across all cancer types.Posted on 09 Feb 2017
Circulating tumor DNA (ctDNA) carrying tumor-specific sequence alterations may provide a minimally invasive means to dynamically assess tumor burden and response to treatment in cancer patients.

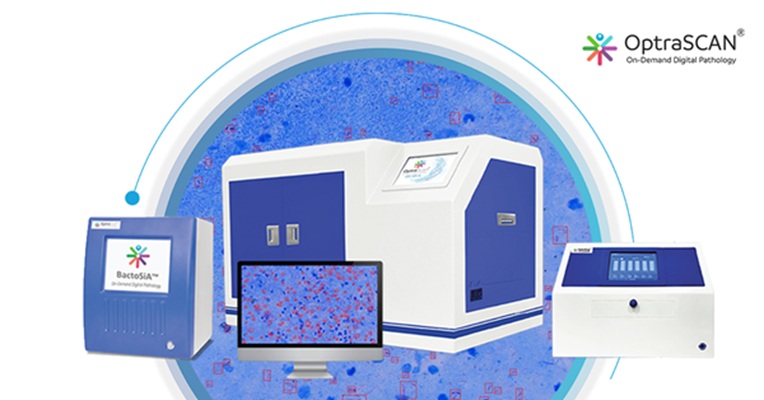
Image: The Biomark microfluidic system for polymerase chain reactions (Photo courtesy of Fluidigm).
Scientists at Cambridge University performed a retrospective analysis of serial plasma samples collected during routine clinical visits from 40 patients with high-grade serous ovarian carcinoma (HGSOC) undergoing heterogeneous standard of care treatment. Patient-specific tumor protein p53 (TP53) assays were developed for 31 unique mutations identified in formalin-fixed paraffin-embedded tumor DNA from these patients.
Digital polymerase chain reaction (PCR) was performed using the Biomark microfluidic system. Total circulating cell-free DNA was measured as the TP53 total allele count (TP53TAC), the sum of estimated targets of mutated and wild-type copies of TP53 amplified by the assay primers. Serum CA-125 level was routinely monitored using a two-site sandwich immunoassay on a Siemens Centaur XP auto-analyzer (upper limit of normal ≤ 30 IU/ml).
The investigators found that the median TP53MAF prior to treatment in 51 relapsed treatment courses was 8% (interquartile range [IQR] 1.2%–22%) compared to 0.7% (IQR 0.3%–2.0%) for seven untreated newly diagnosed stage IIIC/IV patients. The ratio of TP53MAF to volume of disease was higher in relapsed patients than in untreated patients. In 49 treatment courses for relapsed disease, pre-treatment TP53MAF concentration, but not CA-125, was associated with time to progression (TTP). Specificity was improved when patients with recent drainage of ascites were excluded. Ascites drainage led to a reduction of TP53MAF concentration.
The authors concluded that ctDNA is correlated with volume of disease at the start of treatment in women with HGSOC and that a decrease of less than 60% in TP53MAF after one cycle of chemotherapy was associated with shorter TTP. These results provide evidence that ctDNA has the potential to be a highly specific early molecular response marker in HGSOC. James Brenton, MD, a medical oncologist and senior author of the study, said, “Though we’re at an early stage, the results are an exciting signal that levels of faulty DNA in the blood are related to the tumor size, and that changes in these levels could one day be a signpost for doctors and patients to decide if treatment is working for them.” The study was published on December 30, 2016, in the journal Public Library of Science Medicine.