Cytosponge Test Could Replace Uncomfortable Endoscopies
By LabMedica International staff writers
Posted on 23 Nov 2016
A ‘sponge on a string’ pill or Cytosponge test can identify which people with a condition called Barrett’s esophagus who have a low risk of developing esophageal cancer, sparing them uncomfortable endoscopies.Posted on 23 Nov 2016
Barrett's esophagus predisposes to adenocarcinoma, however, most patients with Barrett's esophagus will not progress and endoscopic surveillance is invasive, expensive, and fraught by issues of sampling bias and the subjective assessment of dysplasia.

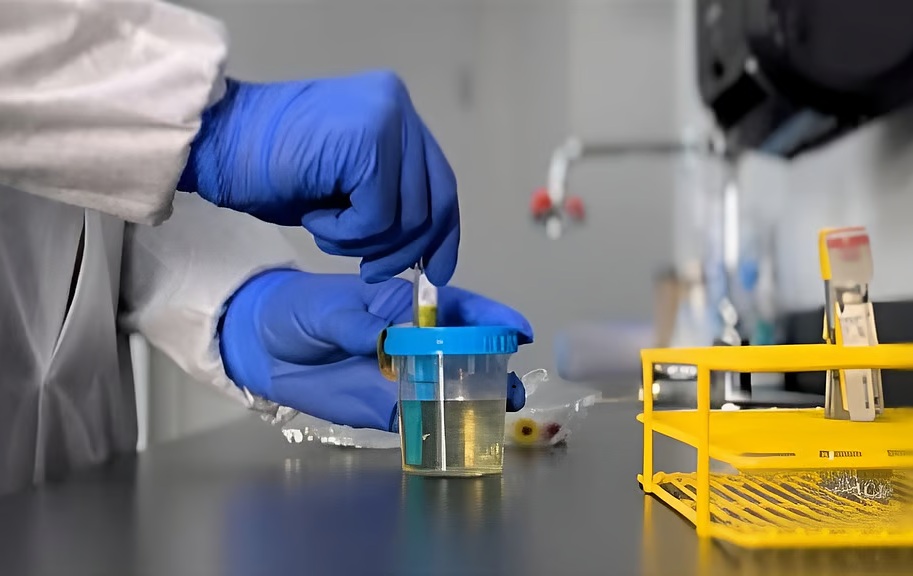
Image: The Cytosponge, a well-tolerated and effective means to sample the lining of the esophagus (Photo courtesy of the University of North Carolina).
A large team of scientists led by those at University of Cambridge (Cambridge, UK) conducted a multicenter cohort study; patients with Barrett's esophagus underwent the Cytosponge test before their surveillance endoscopy. They collected clinical and demographic data and tested Cytosponge samples for a molecular biomarker panel including three protein biomarkers (P53, c-Myc, and Aurora kinase A), two methylation markers Myogenic Differentiation 1(MYOD1) and Runt-related transcription factor 3 (RUNX3), glandular atypia, and tumor protein 53(TP53) mutation status.
The discovery cohort consisted of 468 patients with Barrett's esophagus and intestinal metaplasia. Of these, 376 had no dysplasia and 22 had high-grade dysplasia or intramucosal adenocarcinoma. In the discovery cohort, a model with high classification accuracy consisted of glandular atypia, P53 abnormality, and Aurora kinase A positivity, and the interaction of age, waist-to-hip ratio, and length of the Barrett's esophagus segment.
In the validation cohort of 65 patients, 51 were non-dysplastic and 14 had high-grade dysplasia. In this cohort, 25 (38%) of 65 patients were classified as being low-risk, and the probability of being non-dysplastic was 96.0%. The moderate-risk group comprised 27 non-dysplastic and eight high-grade dysplasia cases, whereas the high-risk group, which was 8% of the cohort had no non-dysplastic cases and five patients with high-grade dysplasia.
The authors concluded that a combination of biomarker assays from a single Cytosponge sample can be used to determine a group of patients at low risk of progression, for whom endoscopy could be avoided. This strategy could help to avoid over diagnosis and overtreatment in patients with Barrett's esophagus. Rebecca Fitzgerald MD, a professor and lead investigator, said, “Most people who have Barrett's esophagus will not go on to develop esophageal cancer, but at the moment there is no way of identifying who will and who won't. Our study is the first step in using the Cytosponge to answer this question.” The study was published on November 10, 2016, in the journal The Lancet Gastroenterology & Hepatology.
Related Links:
University of Cambridge