Tumor Analysis Method Identifies High-Risk Prostate Cancer
By LabMedica International staff writers
Posted on 21 Sep 2016
A new way to identify which prostate cancer patients are likely to develop aggressive types of the disease, even if their tumors at first appear to be lower risk, has been created.Posted on 21 Sep 2016
Prostate cancer is a biologically heterogeneous disease with variable molecular alterations underlying cancer initiation and progression. Despite recent advances in understanding prostate cancer heterogeneity, better methods for classification of prostate cancer are still needed to improve prognostic accuracy and therapeutic outcomes.
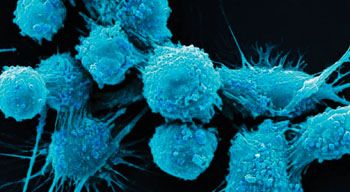
Image: A colorized scanning electron micrograph (SEM) of human prostate cancer cells (Photo courtesy of Dr. Gopal Murti).
A team of scientists led by those at Cedars-Sinai Medical Center (Los Angeles, CA, USA) computationally assembled a large virtual cohort of human prostate cancer transcriptome profiles from 38 distinct cohorts and, using pathway activation signatures of known relevance to prostate cancer, developed a novel classification system consisting of three distinct subtypes (named PCS1–3). They validated this subtyping scheme in 10 independent patient cohorts and 19 laboratory models of prostate cancer, including cell lines and genetically engineered mouse models.
The team found showed that one of the three subtypes of prostate cancer they identified, which they called PCS1, was generally aggressive. In the patients they studied, this subtype showed a high likelihood of spreading and progressing to poor clinical outcomes, including fatalities. Patients experienced poor outcomes even when the tumors had been assigned low Gleason grades. The two other subtypes, PCS2 and PCS3, progressed more slowly. Currently, patients with low-grade tumors often receive no treatment and instead are closely monitored, under a strategy known as active surveillance. The new study indicates active surveillance may not be enough for some of these patients.
An additional advantage to the new subtyping is that it can be performed on tumor cells circulating in the blood. This finding has the potential to improve real-time monitoring of tumor evolution during treatment. Michael Freeman, PhD, the study’s principal investigator said, “About 60% of prostate cancer patients we treat won't progress to aggressive cancer. The problem was that we didn't have a way of knowing which patients fall into that 60%. We hope our findings help physicians provide more patients with optimal treatments, resulting in healthier outcomes.” The study was published on September 1, 2016, in the journal Cancer Research.
Related Links:
Cedars-Sinai Medical Center








 (3) (1).png)