Placental Malaria Diagnosed In Poorly Processed Placental Tissue
By LabMedica International staff writers
Posted on 08 Jun 2016
Placental histopathology has been considered the gold standard for diagnosis of malaria during pregnancy; however, in under-resourced areas placental tissue is often improperly fixed and processed; the resulting formalin pigment is difficult to distinguish from malaria pigment.Posted on 08 Jun 2016
It is often problematic to diagnose malaria in pregnant women because parasitized erythrocytes sequestered in the placenta are often absent from the peripheral circulation. Microscopy of peripheral and placental blood, polymerase chain reaction (PCR), and rapid diagnostic tests have been used but vary in sensitivity and specificity.
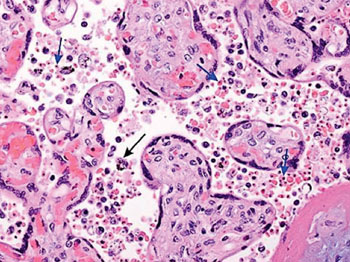
Image: A photomicrograph of placental tissue revealing the presence of the malarial parasites. The blue arrows point to examples of red blood cells containing pigment and the black arrow points to an example of a pigment-containing histiocyte (Photo courtesy of Drucilla J Roberts, MD).
Scientists the University of North Carolina (Chapel Hill, NC, USA) and their international colleagues performed a prospective study and enrolled 182 adult women with healthy, singleton pregnancies less than 23 weeks gestational age. After delivery, a placental biopsy was collected from an incision at a healthy pericentric area of the placenta. Blood samples were collected from study participants zero to 33 days before delivery.
Real-time quantitative polymerase chain reaction (qPCR) was performed on DNA extracted from filter paper-dried blood spots using a high-throughput pooling strategy. Paraffin sections of approximately 5 µm were stained with Giemsa according to standard histologic protocols. The stained sections were examined by two blinded microscopists under light microscopy to assess parasitemia and malaria pigment. Immunohistochemistry (IHC) was using a monoclonal antibody to Plasmodium falciparum histidine-rich protein 2 (HRP2) was carried out on 5 mm thick, formalin-fixed, paraffin-embedded sections using an automated Bond Leica IHC stainer (Leica Microsystems, Bannockburn, IL, USA).
The sensitivity and specificity of individual tests were calculated using PCR or IHC as the reference standard as well as latent class analysis (LCA). The PCR (at time closest to delivery) was used as the gold standard. With PCR as the reference standard, all of the other tests had high specificities, but low sensitivities. The most sensitive other test was IHC, but it missed 50 % of the malaria infections diagnosed by PCR. The correlation between the two blinded microscopists was poor, as there was widespread formalin pigment. Using LCA, all of the tests had high specificities. The most sensitive test was IHC (67.7%), with PCR as second best (56.1%).
The authors concluded that since IHC can detect parasites when they sequester in the placenta but do not circulate, while PCR detects extremely low parasitemia, the combination of both methods might provide a means of detecting the greatest number of infections. Therefore PCR and/or IHC are suitable diagnostics when the presence of formalin pigment substantially compromises placental histopathology. The study was published on May 10, 2016, in the Malaria Journal.
Related Links:
University of North Carolina
Leica Microsystems













