Improved Microscopy May Identify Best Viable Sperm Cells for Reproductive Assistance
By LabMedica International staff writers
Posted on 17 Jan 2016
Researchers’ cutting-edge, stain-free innovation enables more effective screening for and identification of high-quality sperm candidates for assisted reproductive technology (ART).Posted on 17 Jan 2016
Physical, emotional, and financial toll of ART treatments is high because success rates of are still low (20%–30%), so ART is often the last resort for reproductively-challenged couples or individuals. A team of scientists, led by Dr. Natan Shaked, PhD, at Tel Aviv University (TAU; Tel Aviv, Israel) and his MSc student, Dr. Miki Haifler, MD, has devised a new method using interferometric phase microscopy (IPM) that allows analysis without staining, which can affect viability, so sperm cannot be stained if fertilization is the goal as it may result in damaged fetuses. Sperm are nearly transparent under standard microscopy methods; their optical properties differ only slightly from surroundings, resulting in weak image contrast. The challenge is to pinpoint strong sperm candidates without staining, while still being able to characterize viability.
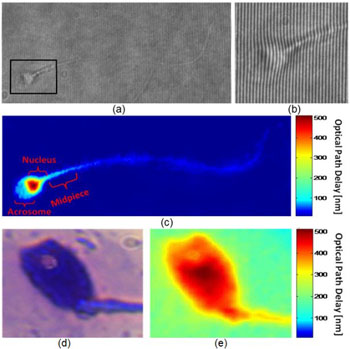
Image: (a) Interferogram obtained using IPM. Sample is still barely seen. However, the OPD information is encoded into the bend of the interference fringes, as can be seen from the enlarged region of interest in (b). (c) The OPD map of the same sperm cell, as digitally calculated from the interferogram shown in (a). All the main morphological features of the cell are discernable. (c, e) Imaging of a sperm cell with an acrosomal vacuole, using: (d) label-based BFM, and (e) label-free IPM. The vacuole is clearly seen as a defect in the OPD map of the IPM image. BFM = bright-field microscopy; IPM = interferometric phase microscopy; OPD = optical path delay (Photo courtesy of Haifler M, Girshovitz P, et al., 2015, and Elsevier publications).
In vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) are two effective ART methods available today. The new method is applicable to both, and is especially helpful in ICSI. "Until now, clinicians have chosen the ‘best’ sperm according to their speed, but speed is not necessarily an indicator of DNA quality," said Dr. Shaked, "Some of the best sperm candidates are slow or even immobile because their tails have malfunctioned. If we can better determine the full structure and composition of the sperm, the success rate of ART treatments will be higher, leading to more births without congenital defects. In cases where sample staining is impossible—such as IVF and ICSI—our device provides a promising new direction."
The new device is a small box that attaches to an existing, even conventional microscope. It is smaller, cost-effective (about USD 1,000), and easier to align than conventional interferometric imaging methods. It is joined to new automated software that produces a thickness map of the sample and other physical parameters to evaluate sperm viability – in real time. The new imaging process, which harnesses phase imaging methods to record passage of light through a sample to assess thickness, can quantify quality of sperm used in ART, leading to more successful treatments.
In the study, to help evaluate the potential of IPM for clinical sperm analysis without staining, the researchers compared label-free IPM to label-free and label-based bright-field microscopy (BFM) in evaluating sperm cell morphology according to World Health Organization (WHO) criteria. Sperm cells from healthy donors were obtained from the male fertility clinic at Chaim Sheba Medical Center (Tel Aviv, Israel). Parameters evaluated were: length and width of the sperm head and midpiece; size and width of the acrosome; head, midpiece, and tail configuration; and general normality of the cell. Results showed that label-free IPM can identify sperm cell abnormalities with excellent correlation compared with label-based BFM, and with higher accuracy compared with label-free BFM. To enable IPM as part of clinical sperm selection procedures, the team is preparing to begin clinical trials on IVF patients in Israel.
The study, by Haifler M, Girshovitz P, et al., was published July 2015, in the journal Fertility and Sterility.
Related Links:
Tel Aviv University