Urine-Based Test Improves Detection of Prostate Cancer
By LabMedica International staff writers
Posted on 02 Jun 2015
A new urine-based test improved prostate cancer detection, including detecting more aggressive forms of prostate cancer, compared to traditional models based on prostate serum antigen, or PSA, levels. Posted on 02 Jun 2015
The test reports individual risk estimates for prostate cancer (PCa) and high grade cancer and each patient's personal threshold for choosing to undergo biopsy may vary, so there is no single cutoff for a "positive" result.
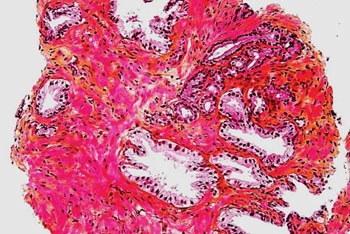
Image: Histopathology of a prostate biopsy showing normal prostatic glands and glands of prostate cancer prostate adenocarcinoma in right upper aspect of image (Photo courtesy of Nephron).
A team of scientists led by those at the University of Michigan Medical School (Ann Arbor, MI, USA) developed the test, which they called Mi-Prostate Score, or MiPS. It combines PSA with two markers for prostate cancer, transmembrane protease, serine 2: V-ets avian erythroblastosis virus E26 oncogene homolog (T2:ERG) and prostate cancer antigen 3 (PCA3), both of which can be detected in a urine sample.
The team studied a total of 1,977 men who were undergoing prostate biopsy because of elevated PSA levels. Using urine samples, the team conducted MiPS testing and compared results to various combinations of PSA, PCA3, T2:ERG and other PSA-based risk calculators. They assessed how well the individual biomarkers and combinations of biomarkers predicted the likelihood of cancer and the likelihood of high-risk cancer, the aggressive type that needs immediate treatment.
Among informative validation cohort samples from 1,225 men, 80% from patients presenting for initial biopsy, models incorporating T2: ERG had significantly greater area under the curve (AUC) than PSA or multivariate Prostate Cancer Prevention Trial risk calculator version (PCPTrc) for predicting or high-grade PCa (Gleason score greater than 6) on biopsy. MiPS models incorporating T2:ERG score had significantly greater AUC than models incorporating only PCA3 plus PSA (or PCPTrc or high-grade cancer PCPTrc [PCPThg]).
Scott A. Tomlins, MD, PhD, assistant professor of pathology and urology and lead author of the study said, “Around 50% of men who undergo a prostate biopsy will not have cancer. We need better ways to manage elevated PSA and determine who really needs to have a biopsy. MiPS gives men and their doctors better information to help make those decisions.” The study was published on May 16, 2015, in the journal European Urology.
Related Links:
University of Michigan Medical School













