Mutations in Rare Asbestos-Caused Cancer Identified by Targeted Next-Generation Sequencing
By LabMedica International staff writers
Posted on 30 Dec 2014
Targeted next-generation sequencing, an advanced genomic analysis tool, was used to identify genes linked to the development of the rare cancer malignant pleural mesothelioma (MPM).Posted on 30 Dec 2014
Malignant mesothelioma is a rare form of cancer that develops from transformed cells originating in the mesothelium, the protective lining that covers many of the internal organs of the body. It is usually caused by exposure to asbestos. The most common anatomical site for the development of mesothelioma is the pleura (the outer lining of the lungs and internal chest wall), but it can also arise in the peritoneum (the lining of the abdominal cavity), the pericardium (the sac that surrounds the heart), or the tunica vaginalis (a sac that surrounds the testis). The three-year survival rate for patients with this disease is only 8%, as most MPM patients are diagnosed with late stage disease with limited therapeutic options.
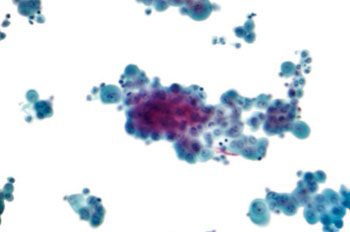
Image: Micrograph of a pleural fluid cytopathology specimen showing mesothelioma (Photo courtesy of Wikimedia Commons).
Investigators at the University of Torino (Orbassano, Italy) used targeted next-generation sequencing (NGS), a method that determines the identity and order of nucleotides in the DNA comprising a specific set of genes rather than sequencing the entire genome, to analyze tumor cells from patients with advanced stage MPM.
In this study, a series of 123 formalin-fixed, paraffin embedded (FFPE) tissue samples with clinical annotations was retrospectively tested with the Life Technologies (Carlsbad, CA, USA) Ion AmpliSeq Cancer Hotspot Panel v.2 library kit to investigate 50 genes plus another two, BRCA1 associated protein-1 (BAP-1) and Neurofibromatosis-2 (NF2), frequently altered in MPM.
Results revealed that mutations clustered in two main molecular pathways, p53/DNA repair and PI3K/AKT (PI3 kinase/protein kinase B). Certain mutations within the PIK3CA, STK11, or TP53 genes associated with a decreased time to disease progression. Additionally, there was a decrease in the time to disease progression and overall survival when there was an accumulation of multiple mutations. Furthermore, a mutation in the BAP-1 gene correlated with nuclear localization of the BAP-1 protein.
Summing up the study, the investigators said, “Our results show that NGS is clearly feasible despite the very well-known challenges of fragmented and low-yield genomic DNA isolated from FFPE tumor tissue. Our data did not identify any specific mutation as a single driver gene, as found in adenocarcinoma of the lung, however our data suggests that in MPM there is an accumulation of several non-driver mutations, which may explain the extremely long latency phase of this asbestos-related disease. Some of the mutations will further be assessed for functional changes and could be carefully considered as stratification factors for future clinical trials investigating the role of targeted-therapies in MPM.”
The study was published in the December 15, 2014, online edition of the Journal of Thoracic Oncology.
Related Links:
University of Torino
Life Technologies