Simple Blood Test Could Improve Treatment for Neuroblastoma
By LabMedica International staff writers
Posted on 28 May 2014
A simple blood test could identify which children are unlikely to respond to treatment for a particularly aggressive form of neuroblastoma, which is the most common extracranial solid cancer in childhood and the most common cancer in infancy.Posted on 28 May 2014
Around 100 children are diagnosed with neuroblastoma in the UK each year, usually in children aged five or under and despite the numbers of children surviving neuroblastoma increasing from around 40% in the 1980s to 60% today, the majority of children have a high-risk form of the disease which is still very hard to treat.
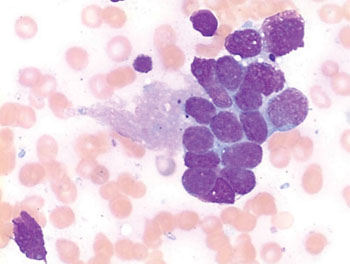
Image: Photomicrograph from a bone marrow aspirate of a cluster of neuroblastoma cells forming the so-called neuroblastoma rosette, typical for this tumor (Photo courtesy of Luhan Swart).
An international team of scientists led by those at the University of Leeds (West Yorkshire, UK) analyzed the levels of three different messenger ribonucleic acids (mRNAs) in blood samples from 290 children taking part in the ongoing Society of Pediatric Oncology trial. Bone marrow aspirates (BM) and peripheral blood (PB) samples were taken from children diagnosed with stage 4 neuroblastoma enrolled between January 2003 and June 2009.
All samples were collected into PAXgene Blood RNA Tubes (PreAnalytiX; Hombrechtikon, Switzerland) and detection of neuroblastoma mRNAs was performed by reverse transcriptase quantitative polymerase chain reaction (RTqPCR). RTqPCR for paired-like homeobox 2b (PHOX2B), tyrosine hydroxylase (TH), and doublecortin (DCX) mRNAs showed that high levels of TH and PHOX2B were found in 19% of the children who died within five years when compared to 38% for the remaining children with low levels of these mRNAs in their blood. There was a higher correlation between the level of mRNAs in BM and the presence of neuroblastoma cells detected by BM cytology and histology at diagnosis.
The authors concluded that high levels of TH and PHOX2B mRNA in PB at diagnosis objectively identify children with ultrahigh-risk disease who may benefit from novel treatment approaches. The level of TH, PHOX2B, and DCX mRNA in BM and/or PB at diagnosis might contribute to an algorithm to improve stratification of children for treatment.
Susan A. Burchill, PhD, the study leader said, “The blood test we are developing can help identify children with the most aggressive form of the disease early on, so they can be offered other experimental treatments. This not only gives them the best chance of living longer, but will help speed up the development of much needed new treatments for this group of children.” The study was published on April 1, 2014, in the Journal of Clinical Oncology.
Related Links:
University of Leeds
PreAnalytiX













