Microfluidic Technology Reveals Early Pancreatic Cancer Biomarker
By LabMedica International staff writers
Posted on 15 May 2014
Cancer cells can be found in the bloodstream in the very early stage of pancreatic cancer, and can be detected before the malignancy is diagnosed.Posted on 15 May 2014
Circulating pancreas cells (CPCs) seed the bloodstream before tumors can be detected using current clinical tests such as computed tomography (CT) and magnetic resonance imaging (MRI) scans, and that detection of pancreatic cells in the blood may be an early sign of cancer.
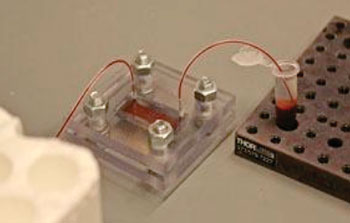
Image: A geometrically enhanced differential immunocapture device (Photo courtesy of Caroline Shin).
Scientists at the University of Michigan Medical School (Ann Arbor, MI, USA) and their colleagues used microfluidic geometrically enhanced differential immunocapture to detect circulating pancreas epithelial cells in 48 patient blood samples. Cyst- and cancer-free patients tended to be younger compared with the cystic lesion and pancreatic ductal adenocarcinoma (PDAC) cohorts. However, there were no differences in other demographics. Most (85%) cystic lesions were classified as side-branch intraductal papillary mucinous neoplasm (IPMNs). The size of cystic lesions varied from 5 mm to 28 mm. Patients with PDAC had a wide range of primary tumor diameters (15 mm to 91 mm) and tumor stages (I–IV).
For this trial, the geometrically enhanced differential immunocapture (GEDI) devices were obtained from AM Fitzgerald and Associates (Burlingame, CA, USA). The active surface of the silicon devices was functionalized with a biotinylated monoclonal antibody for human epithelial cellular adhesion molecule (EpCAM, Santa Cruz Biotechnology; Santa Cruz, CA, USA). Sixteen of 19 cancer-free controls had no CECs by any definition. When CECs were detected, there were no more than three CECs/mL. Seven of 9 (78%) patients with PDAC had detectable CECs, with an average of 16.2 ± 19.5 CECs/mL blood. Eight of 21 (40%) patients with cystic lesions of the pancreas had detectable CECs, averaging 4.5 ± 7.3 CECs/mL blood.
Andrew Rhim, MD, an assistant professor of internal medicine and lead author, said, “While there is much work that still needs to be done, there is great potential for using this technology to identify who is most at risk for developing pancreatic cancer. Studies are underway to interrogate the genomic signature of circulating pancreas cells from patients with precancerous cystic lesions. If these cells represent the earliest forms of cancer, we predict they would possess many of the genetic anomalies we typically see in pancreas tumors.” The study was published in the March 2014 issue of the journal Gastroenterology.
Related Links:
University of Michigan Medical School
AM Fitzgerald and Associates
Santa Cruz Biotechnology