New Testing Method Predicts Trauma Patient Recovery Days in Advance
Posted on 17 Feb 2026
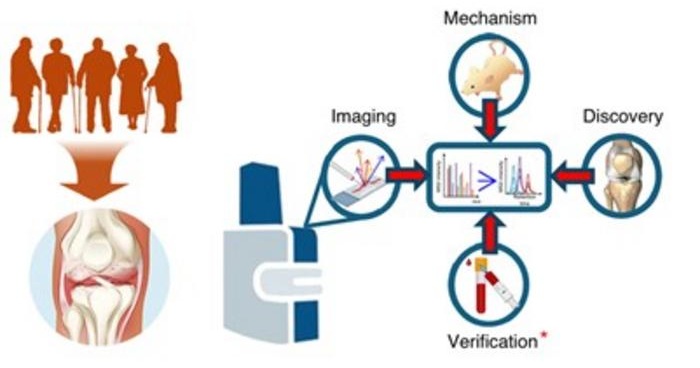
Trauma patients with nearly identical injuries often experience very different recoveries, even when treated similarly. Traditional assessments based on injury severity do not always explain why some patients develop organ failure or die while others recover. This unpredictability limits doctors’ ability to intervene early and tailor care. Now, a new study shows that analyzing molecular signals in blood can predict recovery trajectories and complications days before they appear.
Researchers at the University of Colorado Anschutz Medical Campus (Aurora, CO, USA) conducted a first-of-its-kind study using “omics” technologies, combining proteomics and metabolomics to examine biological signals in trauma patients’ blood. The team mapped molecular endotypes and recovery trajectories in more than 1,300 trauma patients over time. By analyzing patterns of proteins and metabolites, researchers were able to characterize each patient’s biological response to injury rather than relying solely on physical injury scores.

The results showed that organ failure and mortality could be predicted more accurately and efficiently using omics markers than with traditional injury-based measures. The predictive models achieved 92% accuracy and were validated in an independent cohort of more than 300 trauma patients. The findings, published in Science Translational Medicine, demonstrate that molecular profiling can reveal why patients with similar injuries experience different outcomes, enabling earlier and more precise risk assessment.
Researchers say the approach lays the groundwork for personalized trauma care in real-time emergency settings. Efforts are now underway to adapt the molecular profiling system for rapid, point-of-care testing in emergency departments and military environments. The findings are also expected to influence the design of future clinical trials, including a trial evaluating fibrinogen supplementation. Investigators believe this strategy could support the development of targeted therapies and reshape trauma treatment planning.
"Two patients often arrive in the ER with nearly identical injuries but go on to have widely divergent outcomes despite similar care,” said Mitchell Cohen, senior author and professor of surgery at CU Anschutz. “This occurs because their biologic response to injury and treatment is different. Our novel approach and modeling allows us to see those differences in real time, so we can know their biologic state, predict their trajectories and tailor their treatments in a personalized manner.”
Related Links:
CU Anschutz