Simple Method Predicts Risk of Brain Tumor Recurrence
Posted on 17 Feb 2026
Meningioma is the most common type of brain tumor, developing in the membranes surrounding the brain rather than in brain tissue itself. Although often classified as benign, these tumors can cause significant symptoms by pressing on the brain, including headaches and loss of bodily functions. Even tumors categorized as low-risk can recur, creating lasting uncertainty for patients. Researchers now report that examining immune cells within the tumor under a microscope may more accurately predict the risk of recurrence than current classification methods.
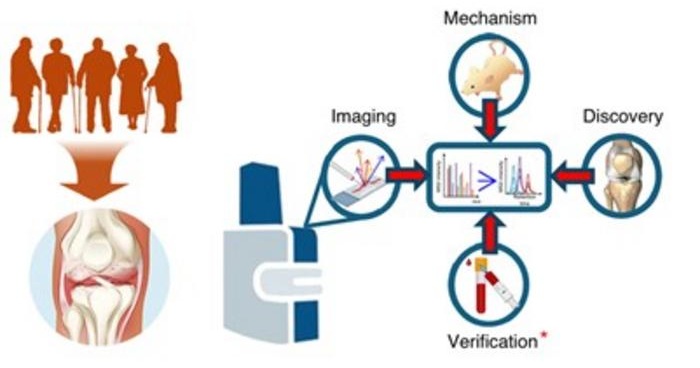
In a study led by Leiden University Medical Center (Leiden, the Netherlands), in collaboration with Heidelberg University (Heidelberg, Germany), and Erasmus MC (Rotterdam, the Netherlands), researchers analyzed DNA profiles from 4,500 meningioma patients, drawing on one of the largest global datasets assembled in Heidelberg. Tumor DNA profiling is widely used to classify meningiomas into risk groups, but it requires advanced and costly techniques. The team investigated whether combining genetic data with microscopic tissue analysis could improve risk prediction in a more accessible way.
The analysis revealed that traditional DNA-based classifications lack clear boundaries in meningiomas, with risk groups overlapping rather than forming distinct categories. When researchers examined tumor samples under the microscope, they found that immune cell patterns provided critical additional insight. Low-risk tumors contained more dormant immune cells, whereas high-risk tumors had fewer immune cells that appeared more active. The findings, published in Nature Genetics, showed that simply counting immune cells predicted recurrence risk more accurately than current microscopic assessments.
The study suggests that immune cell counts could offer a practical, low-cost method for improving risk assessment worldwide. Because pathologists already use similar staining techniques routinely, the approach could be implemented even in settings without advanced genomic technology. Further research will compare the predictive accuracy of immune cell counting against DNA-based tests to determine whether it can replace or complement current methods. Researchers aim to refine recurrence prediction models in the coming years to reduce uncertainty for patients.
“With a simple and inexpensive technique that pathologists already use every day, it’s now possible make a better risk assessment, even in countries where advanced technologies are not available,” said neuropathologist Niek Maas, co-author of the study. “Further research is needed to compare the accuracy of these predictions. We will be working on this intensively in the coming years.”
Related Links:
Leiden University Medical Center
Heidelberg University
Erasmus MC