Blood Test Could Help More Women Survive Aggressive Triple Negative Breast Cancer
Posted on 12 Mar 2025
Cancer research shows that over 90% of women diagnosed with breast cancer at its earliest stage survive for five years or more. However, this survival rate dramatically decreases to just 30% when the cancer is discovered at more advanced stages. One of the challenges in treating breast cancer, particularly aggressive forms such as triple-negative breast cancer, is the difficulty in quickly assessing treatment effectiveness. Often, doctors rely on chemotherapy regimens, which are expensive and toxic, continuing with treatment even when it proves ineffective. Typically, doctors cannot determine if a chemotherapy regimen is working until the patient has completed all the prescribed cycles, which can take up to six months. If the treatment is unsuccessful, the patient may need to begin a new regimen, starting the process over. Now, a simple blood test that searches for a biomarker in plasma will allow doctors to assess quickly whether cancer treatments, like chemotherapy, are working. This allows for faster adjustments to the treatment plan, switching to more effective therapies if necessary.
Previously, researchers have focused on nitric oxide production, a molecule that regulates cancer cell growth. Researchers at the University of New England (UNE, Portland, ME, USA) discovered a biomarker called Nw-hydroxy-L-Arginine (NOHA) that is a sensitive and reliable indicator for estrogen receptor-negative tumors, which are more aggressive types of breast cancer. Prior research had already linked nitric oxide, inflammatory biology, and breast cancer. The researchers realized that NOHA, being upstream of the nitric oxide process, could be measured through a blood test rather than a tissue sample. NOHA directly correlates with nitric oxide levels, without interference from other biological pathways. With this discovery, they began exploring NOHA as a biomarker for both detecting and monitoring breast cancer and even applied for a patent for a diagnostic tool that uses this blood marker to track aggressive, estrogen-negative tumors.
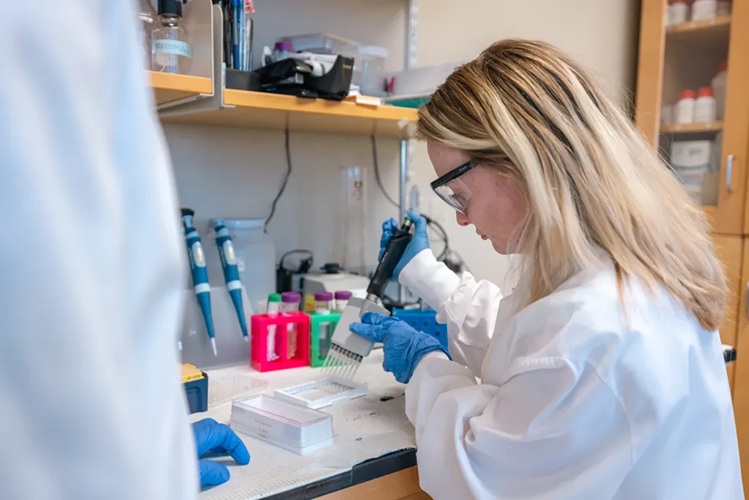
The researchers conducted a study in Tanzania to test whether NOHA could determine the estrogen receptor status in breast cancer patients. The results from this study were promising, suggesting that NOHA has the potential for improving cancer care. With the NOHA blood test, doctors could monitor NOHA levels after each treatment cycle. If the levels show an unfavorable change, the physician could pause the current drug combination and try another. Building on these findings, the team is now researching NOHA's role in managing triple-negative breast cancer in the U.S. through clinical trials, which are essential in translating laboratory results into real-world applications.
In addition, the team is exploring NOHA’s potential for early detection of breast cancer, particularly for individuals with genetic predispositions, and its role in drug development. Their work is setting the stage for more dynamic monitoring of treatment effectiveness. Following their success with breast cancer, the researchers have expanded their work to ovarian cancer. The American Cancer Society estimates that nearly 20,000 new cases of ovarian cancer will be diagnosed in the U.S. this year, with almost 13,000 women dying from the disease. Because the symptoms of ovarian cancer are often subtle or absent in its early stages, the disease is frequently diagnosed at a later, more advanced stage. The researchers' findings indicate that NOHA could also be used to detect and monitor ovarian cancer. This led them to secure a second patent for a blood diagnostic tool to identify ovarian cancer, broadening the impact of their groundbreaking research.
“It validates to us that (NOHA) is not only going to be centric to breast cancer, but it can also expand to other tumors like ovarian cancer,” said Srinidi (Sri) Mohan, Ph.D., professor at the University of New England School of Pharmacy, who identified NOHA as a potential biomarker for breast cancer detection and monitoring.
Related Links:
University of New England