Diagnostic Test Could Detect Elusive Neuro Disorder Using Tiny Drop of Spinal Fluid
Posted on 08 Jul 2024
Progressive supranuclear palsy (PSP) is a severe neurological disorder classified under frontotemporal dementia (FTD) that impairs cognition, movement, and behavior. Thought to be caused by an accumulation of tau proteins that damage and kill cells, PSP presents symptoms such as poor balance with frequent backward falls and difficulties moving the eyes vertically. Often misdiagnosed as Parkinson’s disease, PSP progresses more rapidly and does not respond to Parkinson’s treatments. Most individuals with PSP pass away approximately seven years after symptoms begin, and frequently, the disease is only identified posthumously during an autopsy. Unlike Alzheimer’s, there are no tau scans, blood tests, or MRIs that can conclusively diagnose PSP, a fact that has hampered the development of treatments. Now, the discovery of a unique pattern of proteins in the spinal fluid of patients could lead to earlier diagnosis and the development of new treatments for PSP.
In a study published in Neurology on July 3, researchers at the UCSF Department of Neurology (San Francisco, CA, USA) discovered a unique protein pattern in the spinal fluid of PSP patients. This finding was achieved using a novel high-throughput technology capable of analyzing thousands of proteins from just a small fluid sample. The researchers are optimistic that these protein biomarkers might lead to a diagnostic test and therapies aimed at halting the disease's deadly progression. Previous studies have noted the potential of various non-specific neurodegeneration biomarkers in PSP, though they have shown limited sensitivity and specificity, especially in the early stages of the disease. In this latest research, protein biomarkers were quantified using high-throughput technology, which utilizes molecules that bind selectively and specifically to proteins.
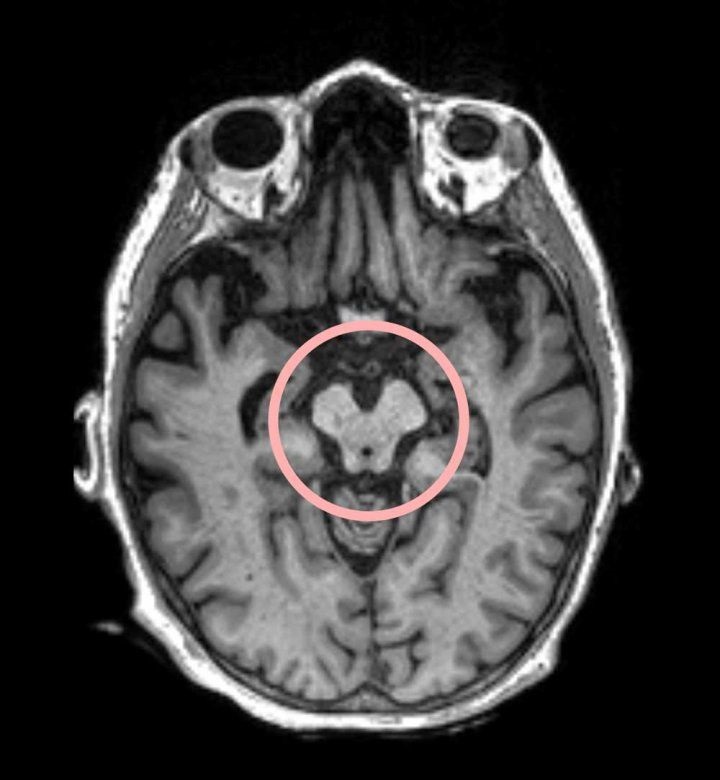
The study involved 136 participants, averaging 70 years of age, including patients from UCSF and other institutions showing symptoms consistent with PSP, as well as autopsy-confirmed PSP cases. Researchers compared biomarkers from these individuals to those from healthy controls and patients with other types of FTD. They observed generally lower protein levels in those with confirmed or suspected PSP compared to healthy study participants. The protein profile in autopsy-confirmed PSP cases also varied distinctly from those with other FTD forms and living patients. Notably, all individuals with confirmed or suspected PSP exhibited elevated levels of proteins linked to neurodegeneration. Additionally, certain inflammatory proteins were identified that correlated with disease severity, alongside a decrease in proteins vital for various brain cell functions, offering potential targets for future therapeutic interventions.
“This work aims to create a framework for using these newly identified proteins in future clinical trials,” said first author, Amy Wise, formerly of the UCSF Department of Neurology, and the Memory and Aging Center, and currently a medical student at UC Davis. “We hope to reach a point where a single biomarker, or a panel of biomarkers from a blood test or lumbar puncture, can provide definitive diagnostic and prognostic results for PSP.”
Related Links:
UCSF Department of Neurology