Noninvasive Liquid Biopsy Test for Advanced Melanoma Can Track Treatment Response and Tumor Recurrence
Posted on 09 Oct 2023
Circulating tumor DNA (ctDNA) is gaining attention as a blood-based biomarker for various types of solid tumors, including melanoma. For those with BRAF wild-type (BRAF WT) stage III and IV melanoma, there is a pressing need for markers that can predict how the disease will progress and how well treatments are working. While many late-stage melanoma patients have a specific BRAF mutation that responds well to certain drugs, those with BRAF WT or different BRAF variants do not get the same benefits from combined immune checkpoint inhibitor (ICI) therapies.
A new study by researchers from The University of Queensland (Brisbane, Australia) evaluated the utility of ctDNA levels in the blood of patients with BRAF WT stage III and IV melanoma. Their aim was to discover any genetic variants in the blood that could lead to alternative treatments and improved patient outcomes for BRAF WT patients. They found that changes in ctDNA, which is released into the blood by dying tumor cells, can be monitored through non-invasive tests.
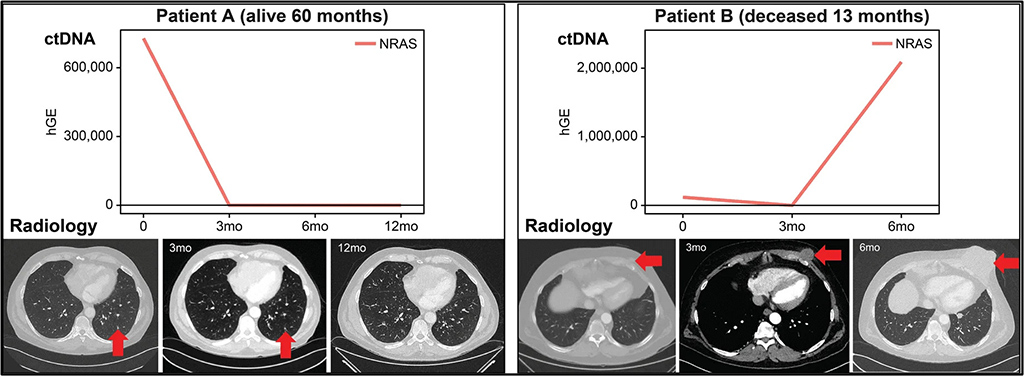
In the study, researchers examined ctDNA levels from the plasma samples of 106 patients. Additionally, serial blood samples from a subgroup of 16 patients were used for a more extended study. Remarkably, they found variants in 85% of patients, all of which were in pathways that could be targeted for treatment. The level of ctDNA in the blood also had predictive value; stage IV melanoma patients with ctDNA levels below 10 ng/mL showed significantly better disease-specific and progression-free survival rates. On the other hand, patients with both high levels of ctDNA and detectable variants had the poorest outcomes. Furthermore, longitudinal changes in ctDNA levels over time were found to be in line with treatment response and disease progression determined by radiology assessments.
The findings support the use of ctDNA as a non-invasive "liquid biopsy" for identifying recurrent disease and targetable genetic variants in late-stage melanoma patients. Using ctDNA as a clinical tool is particularly appealing because it provides repeatable, non-invasive tests that can offer valuable insights into treatment efficacy and disease recurrence. The study showed the significance of ctDNA in stage IV melanoma patients for identifying somatic variants with clinically targetable mutations, as a prognostic indicator in patients with stage IV melanoma, and as a tool for monitoring treatment response to ICI therapy.
“Our results showed that changes in ctDNA over time correlated with response to treatment and progression of the disease as assessed by radiology. Measuring patients’ ctDNA throughout their treatment would help follow their potential response and adapt the treatment regimen accordingly,” said lead investigator Vanessa F. Bonazzi, PhD. “While patients can have a PET/CT scan every six months, a blood test could be performed monthly and provide an accurate answer followed by immediate actions. If for example, the patient ctDNA profile shows a PIK3CA mutation from baseline, you could follow it in different blood samples from this patient over time, and down the track, you could use a PIK3CA inhibitor and hopefully be able to prevent potential recurrence of disease.”
Related Links:
The University of Queensland














