New Technique Enables Measurement of Thousands of Molecules from Single Blood Drop
Posted on 26 Jan 2023
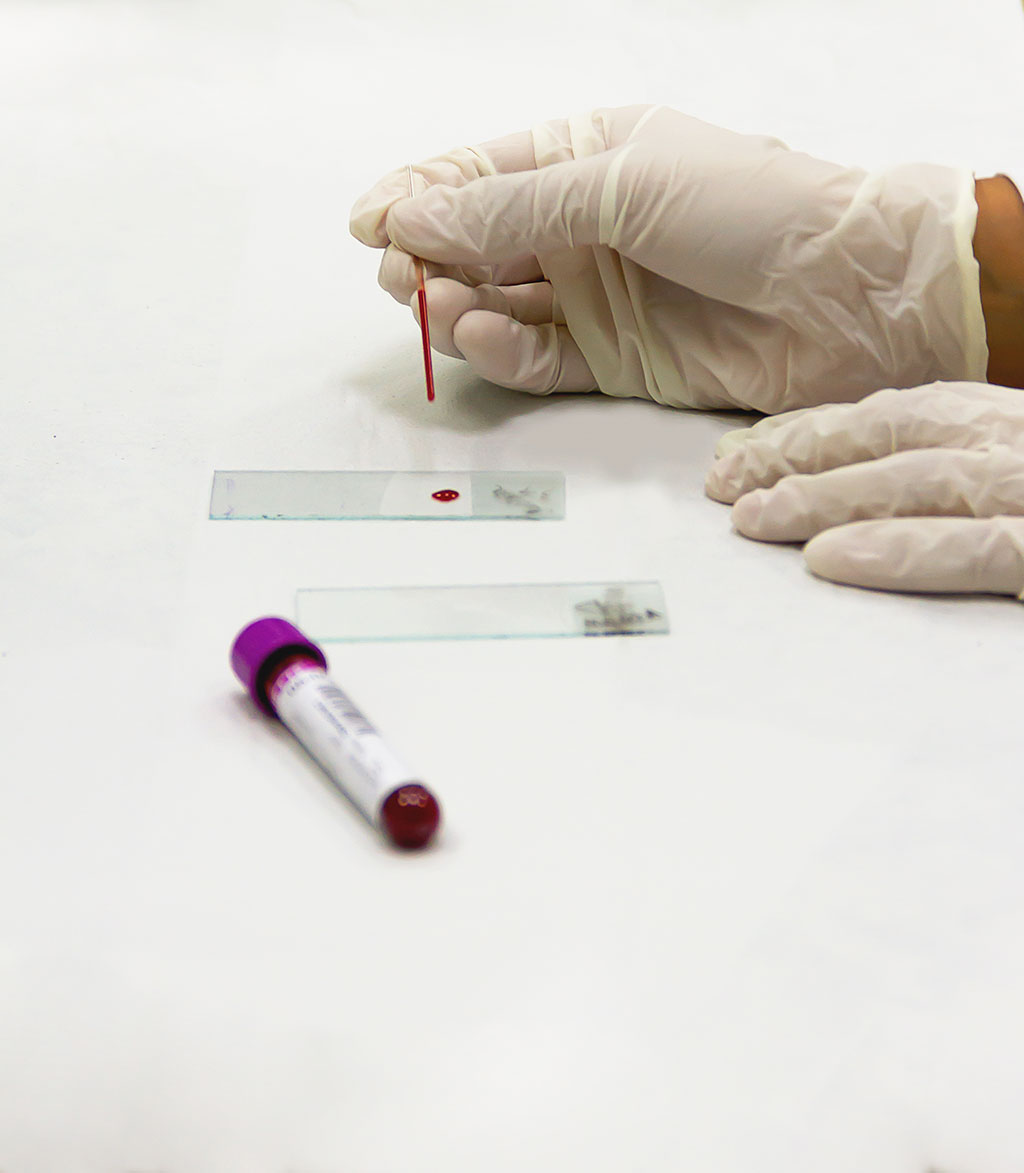
“Multi-omics” technologies are capable of simultaneously analyzing various proteins, fats, by-products of metabolism and inflammatory markers. While finger-prick testing for diabetes measures a single type of molecule (glucose), multi-omics microsampling provides data regarding thousands of different molecules at once. Rather than focus on any single protein, metabolite or inflammatory marker, “omics” research adopts a broader, systems-biology approach by analyzing the entire spectrum of proteins (the proteome), fats (the lipidome) or the by-products of metabolism (the metabolome). Some recent advances have made this data analysis more robust and efficient, although the real-world usefulness of “multi-omics” research has been limited by various challenges, particularly the difficulties in sample collection. Several samples may be required to be taken within a short time span in order to measure a person’s response to a food or medication. Presently, sampling requires a person to travel to a clinic for an intravenous blood draw of 10 to 50 milliliters. Now, that could change after researchers have shown that they can measure thousands of molecules from a single drop of blood by using a new approach that combines a microsampling device with “multi-omics” technologies.
Researchers at Stanford Medicine (Stanford, CA, USA) set out to investigate whether it was possible to sharply reduce the volume of blood required for “multi-omics” analysis, but could still profile thousands of molecules. For their study, the researchers chose a microsampling device called Mitra, a portable finger-stick device that draws 10 microliters of blood into a gel matrix, and went on to test multiple extraction techniques for separating out the proteins, lipids and metabolites. In order to measure the inflammatory markers, the researchers used a second separate microsample. In a pilot study involving two test subjects, the researchers managed to measure the levels of 128 proteins, 1,461 metabolites and 776 lipids from each microsample. The team also monitored the samples for stability after storing them at various temperatures and found very few proteins to be unstable, irrespective of the temperature levels. They found that some lipids and metabolites broke down during storage at particular temperatures, although most of them remained stable.
A comparison of the “multi-omics” results obtained through microsampling with those from a traditional blood draw revealed similar results from the two collection types for most of the molecules. The researchers now became confident of the reliability of their multi-omic microsamples and went on to test the applications for the new technique. They analyzed data from 28 subjects for four hours after they had consumed a specific quantity of carbohydrates, fats, proteins and micronutrients from a meal replacement shake to monitor its molecular impact. The researchers found that people responded differently to the mixture. While people can have very different metabolic responses to the same food, standard blood tests are unable to provide sufficient data to understand why this is so.
The researchers eventually detected almost 50% of the compounds in the shake in the blood of the participants. After dividing the participants into two groups based on how quickly the molecules changed in their blood, the team found that one group responded more quickly to the shake than the other. Participants diagnosed with insulin resistance were more likely to come under the “fast responder” group. Some participants also exhibited an inflammatory reaction, with the molecules involved in their immune response peaking about 30 minutes after consumption of the shake. In a second experiment, the team sampled a researcher’s blood after every one to two hours while he was awake for a week. At the end of the week, the team had made 214,661 biochemical measurements, including levels of proteins, fats and hormones such as cortisol, which were compared with physiologic data obtained from wearable sensors.
The researchers observed that several molecules exhibited previously unidentified 24-hour rhythms (or certain molecules followed a daily, cyclic ebb and flow), while there were extensive variations in glucose and cortisol levels throughout the day, in contrast to their expectations. The researchers now plan to expand the pilot studies and offer multi-omic microsampling to a broader patient group. The researchers believe that in the future, healthy people could perform multi-omic microsampling at home every month, every week, or once a day to obtain a sense of their personal molecular fingerprint. Any subtle changes in this fingerprint could indicate the onset of a disease much before standard lab tests picked up any abnormality.
“The most exciting thing about microsampling is the ability to collect denser time points and more comprehensive data,” said Ryan Kellogg, PhD, post-doctoral researcher in genetics and one of four co-lead authors on the paper. “With traditional venipuncture, your doctor gets a sample every six months, or maybe even every few years. There’s a lot of biology happening between those samples.”
“Several ongoing projects are evaluating if this method can be used for early disease detection,” said Stanford postdoctoral scholar Xiaotao Shen, PhD, who was in charge of data analysis for the project. “Through longitudinal monitoring, we’re very hopeful this can be used for diagnosis.”
Related Links:
Stanford Medicine














