Single Blood Test Predicts Risk of Multiple Diseases Simultaneously Using AI
Posted on 27 Sep 2022
Prevention is better than cure. To prevent diseases from occurring in the first place, it is important to identify those individuals who are at particularly high risk as early as possible. Yet current screening methods are often costly and focus only on one disease at a time. Now, scientists have profiled 168 metabolic markers in the blood samples of over 100,000 people and combined this data with their medical histories. With the help of artificial intelligence (AI), they were able to predict the risk of onset of several diseases with just one test and show where early intervention could be beneficial.
Scientists from the Berlin Institute of Health at Charité (BIH, Berlin, Germany), Charité – Universitätsmedizin Berlin (Berlin, Germany), and University College London (London, UK) began to delve into the massive treasure trove of data in the UK Biobank. The British study has been tracking more than 500,000 participants for over 15 years. As all Britons have had an electronic health record since the 1990s, these anonymized data allows for the observation of disease development over long periods of time. Recently, the UK Biobank made an enormous data package available to researchers: participants’ frozen blood samples, some of which were more than 15 years old, had been analyzed to measure their levels of 168 metabolites using nuclear magnetic resonance (NMR) spectroscopy. This method is considered robust, easy to perform, and relatively inexpensive. It measures the levels of substances like cholesterol and blood sugar, but also molecules that are lesser known and less frequently identified in blood tests.
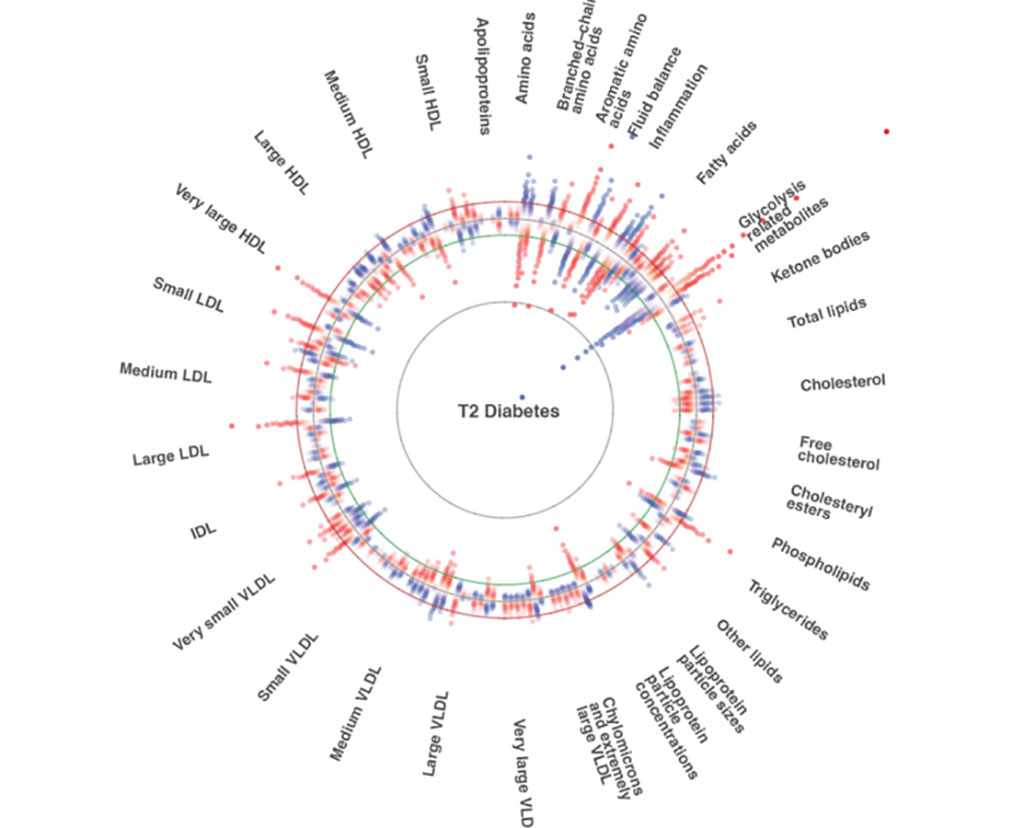
The scientists examined the participants’ data for 24 common diseases – including metabolic disorders like diabetes, cardiovascular diseases like heart attacks and heart failure, musculoskeletal diseases, a variety of cancers, and neurological diseases like Parkinson’s. They determined which participants had contracted any of the 24 diseases in the course of the study and combined this information with the composition of metabolites in their blood (the blood metabolome) from a sample that had been taken before the onset of the disease. With this information, they then turned to AI to create a model that is able to calculate the extent to which the blood’s metabolomic state predicts the development of a future disease.
“We tested the metabolomic profiles for their predictive power and compared these results with conventional methods for calculating disease risk,” said Thore Bürgel, a doctoral student at the BIH’s Digital Health Center and co-first author of the paper along with Jakob Steinfeldt. “We found that our profiles improved risk prediction for the majority of the diseases studied when we combined them with information about the age and sex of the participants.”
The combination of age, sex, and metabolomic state was able to predict the risk of diabetes or heart failure, for example, better than established clinical predictors that measure sugar or cholesterol in the blood. And with a cost of under Euro 20, examining the metabolome is also relatively inexpensive. The scientists have gone one step further with their model and calculated the thresholds that could signal when preventive interventions would be advisable. Specifically: At what thresholds does the new method best identify those who could be saved from heart failure, for example, through the use of medication?
“Again, we saw that metabolomic profiling combined with information on age and sex was as good as or even better than conventional analyses at identifying patients who could benefit from preventive intervention in the form of medication or lifestyle changes,” said Prof. Roland Eils, founding director of the BIH’s Digital Health Center. “We have since been able to successfully validate our model in four other cohort studies conducted in the Netherlands and the UK, indicating that our models are broadly applicable.”
Related Links:
BIH
Charité – Universitätsmedizin Berlin
University College London













