Gene Deletion Underlies Resistance to Chemotherapy in Triple-Negative Breast Cancer
Posted on 30 Aug 2022
A proteognomics approach was used to identify biomarkers in samples from triple negative breast cancer (TNBC) patients that were associated with resistance to chemotherapy treatment.
Proteogenomics is a field of biological research that utilizes a combination of proteomics, genomics, and transcriptomics to aid in the discovery and identification of peptides. Proteogenomics is used to identify new peptides by comparing MS/MS spectra against a protein database that has been derived from genomic and transcriptomic information.
Triple-negative breast cancer (TNBC) is a type of breast cancer that lacks or shows low levels of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) overexpression and/or gene amplification. TNBC comprises 15–20% of all breast cancer cases and affects more young women or women with a mutation in the BRCA1 gene than other breast cancers. Triple-negative breast cancers, which comprise a very heterogeneous group of cancers, are the most challenging breast cancer type to treat, as hormone therapy that is used for other breast cancers does not work for TNBC.
In its early stages, TNBC is typically treated through surgery, radiation, and chemotherapy. In later stages where surgery is not possible or the cancer has spread from the initial localized area, treatment is limited to chemotherapy and in some cases further targeted therapy. Triple-negative breast cancers have a relapse pattern that is very different from hormone-positive breast cancers where the risk of relapse is much higher for the first three to five years, but drops sharply and substantially below that of hormone-positive breast cancers afterwards.
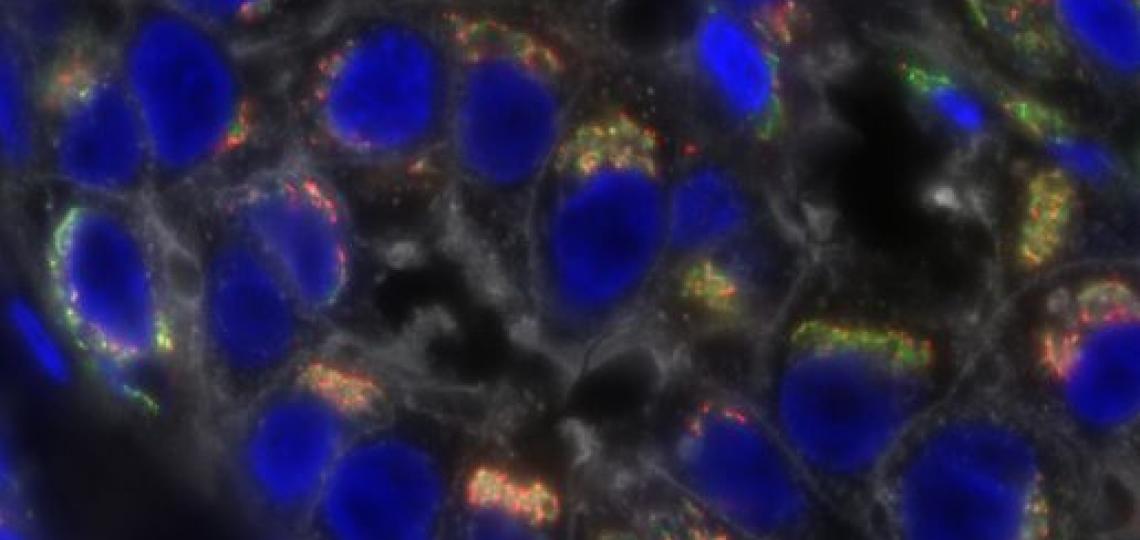
In order to predict response to treatment, investigators at Baylor Medical College (Houston, TX, USA;) and their colleagues used an innovative analytic approach called “microscaled proteogenomics” to analyze tumor biopsies taken from TNBC patients prior to treatment with carboplatin and docetaxel combination chemotherapy. Data from standard DNA and RNA sequencing approaches were integrated with mass spectrometry-based proteomics and phosphoproteomic analyses to derive more complete molecular portraits of treatment-responsive versus treatment-resistant tumors.
Results of proteogenomic analyses of somatic copy number aberrations identified a resistance-associated 19q13.31-33 deletion where the genes LIG1, POLD1, and XRCC1 are located. LIG1 (DNA ligase I) gene deletion and/or low mRNA expression levels were associated with lack of pathological complete response, higher chromosomal instability (CIN), and poor prognosis in TNBC, as well as carboplatin-selective resistance in TNBC pre-clinical models. Hemizygous loss of LIG1 was also associated with higher CIN and poor prognosis in other cancer types, demonstrating broader clinical implications.
“TNBC is the most difficult to treat form of breast cancer, with standard treatment requiring multiple chemotherapy drugs that unfortunately often fail to cure the patient,” said first author Dr. Meenakshi Anurag, assistant professor of medicine at Baylor Medical College. “It is imperative that we develop approaches to predict response so that only effective treatments are given. Furthermore, patients who do not respond to standard drugs need entirely new treatment approaches. The discovery of therapeutic alternatives will depend on new insights into how TNBC arises.”
The study was published in the August 24, 2022, online edition of the journal Cancer Discovery.














