Mutation Testing Utilized in Anaplastic Thyroid Cancer
Posted on 26 Aug 2022
Mutations in two key oncogenes are associated with patient outcomes in anaplastic thyroid carcinoma (ATC), pointing to the utility of tumor mutation testing during treatment decision making for individuals with the disease.
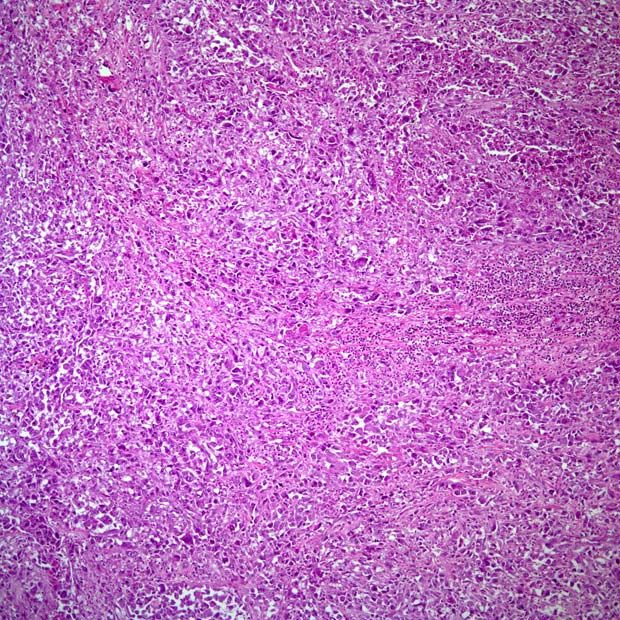
ATC, a rare but deadly form of thyroid cancer, has been shown to be genetically heterogeneous, but the clinical significance of the cancer's different mutation profiles has not been closely examined. ATC is characterized by advanced disease at presentation and rapid progression within weeks.
Medical Oncologists at the University of Texas MD Anderson Cancer Center (Houston, TX, USA) and their associates performed mutation sequencing using targeted gene panels on 202 ATC patients and found that the cancer can be divided into three subtypes based on mutually exclusive driver mutations in the genes BRAF and RAS.
Tumor materials obtained from fine needle biopsy, core biopsy, excisional biopsy, or surgical resection were used for mutational testing. Paired stained slides were used to identify tumor regions of interest and assess for tumor cellularity (>20%). NGS was performed with a minimum depth of approximately 250×. Where blood samples were available, gene panels incorporating germline variant subtractions were used including Solid Tumor Genomic Assay V1 (128 genes), Solid Tumor Genomics Assay 2018 (134 genes), and MDA-409 (409 genes) which detected SNVs and indels. NGS of liquid biopsy samples was performed on circulating cell free DNA (cfDNA) using a validated 70-gene panel (LB70), which detects SNVs and indels in 70 genes.
The investigators reported that a total of 202 patients were included, and 122 died of ATC (60%). The median follow-up was 31 months (interquartile range, 18-45 months). The most common mutations were in TP53 (59%), BRAF (41%), TERT promoter (37%), and the RAS gene family (22%). Clinicopathologic characteristics and overall survival (OS) significantly correlated with mutations in BRAFV600E and RAS, which were mutually exclusive. The BRAFV600E mutation was associated with the presence of a papillary thyroid carcinoma precursor and significantly better overall survival (median OS: 24 months). RAS-mutated patients more commonly presented without cervical lymph node involvement, but had the worst OS (median OS: 6 months). Tumors that were wild-type for both BRAF and RAS were enriched for NF1 mutations and harbored intermediate prognosis (median OS: 15 months).
The authors concluded that driver mutations in ATC are associated with distinct clinicopathologic features and survival outcomes, reflecting heterogeneity in tumor biology. Although treatment with BRAF/MEK inhibitors can be initiated on the basis of knowledge of BRAFV600E status alone (i.e., using immunohistochemistry), knowledge of RAS and TP53 mutation status allows for additional risk stratification and can guide further therapeutic decision making. As such, comprehensive tumor mutation profiling should be obtained for patients with ATC as a part of the routine clinical workup at diagnosis. The study was published on August 17, 2022 in the journal JCO Precision Oncology.














