New State-of-the-Art, Ultrasensitive Blood Test to Transform Detection of Brain Damage and Poor Prognosis After Head Injury
Posted on 06 Oct 2021
A new study has used a state-of-the-art blood test to track damage to the brain in people who have sustained traumatic brain injury (TBI).
The study by researchers from the UK DRI Care Research and Technology Centre, based at Imperial College London (London, UK) found that measuring the protein biomarker in the blood can provide a simpler, more accurate way to predict clinical outcomes and help to identify those at higher risk of developing dementia. Around 50 million people each year worldwide experience TBI as a result of head injury. In the brains of these individuals, the neurons encounter severe stretching and sheering forces which cause damage to their axons, the part which transmits electrical signals. Axonal damage is the best predictor of clinical outcomes and recovery but has been difficult to measure in patients.
The research team set out to identify a chemical that could be easily detected in the blood - a biomarker - that would accurately reflect this axonal damage in the brain after TBI. A multicentre study was established involving over 200 patients who had experienced moderate to severe TBI, recruited from eight major trauma centers across Europe. In 56% of cases the injuries were classed as ‘high energy’, involving falls from over 3 meters or collisions at more than 30km/hour, with the majority of these caused by road traffic accidents.
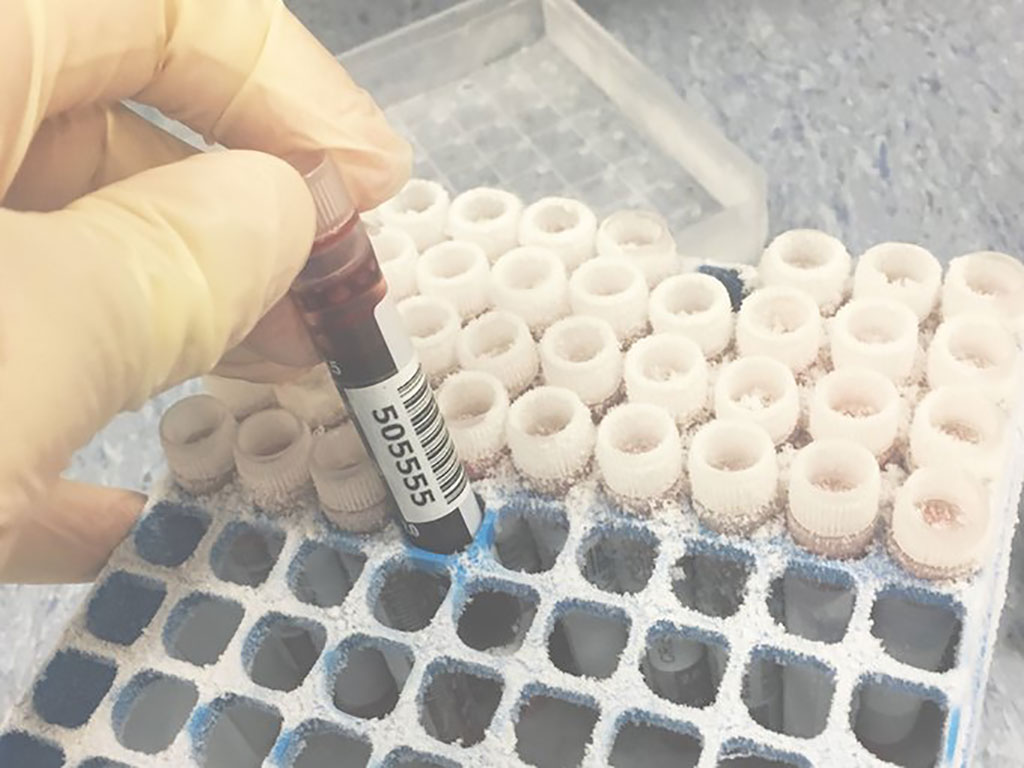
To find a suitable protein marker, the researchers harnessed cutting-edge technology called single molecule array (SiMoA) that can measure sub-femtomolar (10-16) levels of chemicals in the blood. Starting their search by detecting proteins that are important to the structure of the axons, they found that measuring blood levels of neurofilament light provided a remarkably accurate long-term prognosis for the patient. Neurofilament light has become a useful tool for diagnosis, monitoring and prognosis across neurodegenerative disease like Alzheimer’s, but its potential for use in TBI has not been fully assessed and optimised until now.
The team also used advanced types of brain imaging to validate blood test findings. Blood levels of neurofilament light were found to be closely related to measures from diffusion MRI, an advanced type of imaging which also provides measures related to damage to axons. The team also compared blood levels of neurofilament light with a special type of brain imaging that measures shrinkage (atrophy) of the brain, indicating the loss of nerve cells. They found that blood levels of neurofilament light tracked extremely well to brain atrophy and importantly predicted further nerve cell degeneration up to one year after the injury. These findings mean future blood tests could provide similar information to MRIs, but in a more cost-effective and accessible manner.
In order to further validate the blood biomarker findings, the team also analyzed fluid samples from around the damaged neuronal axons. Following surgery in some of the patients, such as a craniotomy to remove part of the skull, the team inserted catheters into the brain. With simultaneous measurements taken from the blood, the researchers were able to identify a strong correlation, supporting evidence that the protein in the blood originated at the source of the damage, and so reflected well the progressive damage taking place in the brain.
“Outcomes after TBI are very difficult to predict. This is a major challenge for doctors trying to care for patients recovering from head injuries of all severities,” said Prof David Sharp, Director of the UK DRI’s Care Research and Technology Centre. “What we need are more accurate diagnostic tests that can be used in our major trauma units and clinics. Our work shows that measuring neurofilament light soon after head injury helps predict who will develop long-term problems. We are applying this in various contexts, including for the investigation of sporting TBI, and will be investigating whether this blood test can be used to predict those at high risk of developing dementia”
“Traumatic brain injury is a risk factor for dementia, and identifying the long-term impact of individual head injuries remains an important goal for research,” said Dr. Rosa Sancho, Head of Research at Alzheimer’s Research UK. “This work gets us closer to a blood test able to predict how brain changes develop up to one year after injury. Dementia develops over many years and we need to build on these findings to help improve longer-term prognosis and to reliably determine an individual’s risk of dementia following a head injury.
Related Links:
Imperial College London













