Liquid Bioassay for Ultrasensitive Detection of Circulating HPV DNA
By LabMedica International staff writers
Posted on 04 Oct 2021
A recent paper concluded that for cancers caused by the human papillomavirus (HPV), the HPV-seq technique was a promising ultrasensitive approach for detection and analysis of circulating tumor DNA (ctDNA).Posted on 04 Oct 2021
HPV DNA offers a convenient ctDNA marker for HPV-associated cancers, but current methods such as digital PCR (dPCR) provide insufficient accuracy for clinical applications in patients with low-disease burden. In this light, investigators at Princess Margaret Cancer Centre (Toronto, Canada) asked whether a next-generation sequencing approach (HPV-seq) could provide quantitative and qualitative assessment of HPV ctDNA in low-disease-burden settings.
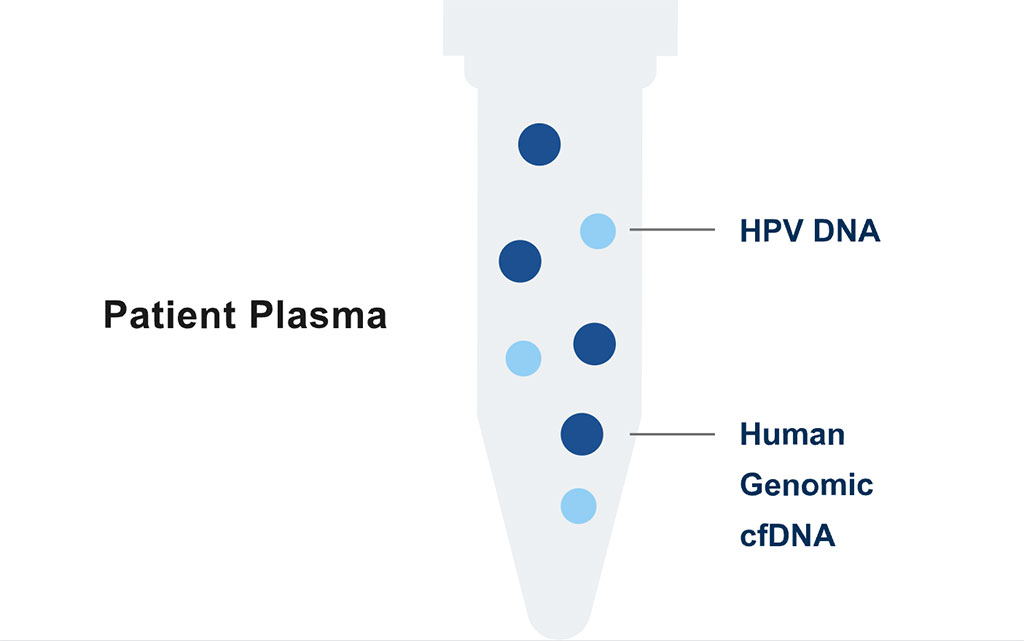
Image: The HPV-Seq test is an ultra-sensitive liquid biopsy solution for the identification and quantification of circulating HPV 16 and HPV 18 DNA in patients with cancers caused by HPV infection (Photo courtesy of Sysmex Inostics)
The classical PCR test carries out one reaction per single sample. The digital PCR (dPCR) method also carries out a single reaction within a sample, however the sample is separated into a large number of partitions and the reaction is carried out in each partition individually. This separation allows a more reliable collection and sensitive measurement of nucleic acid amounts. The dPCR method has been demonstrated as useful for studying variations in gene sequences - such as copy number variants and point mutations - and it is routinely used for clonal amplification of samples for next-generation sequencing.
The HPV-seq test is an ultra-sensitive liquid biopsy approach for the identification and quantification of circulating HPV 16 and HPV 18 DNA in patients with cancers caused by HPV infection, including cervical cancer, anal squamous cell carcinoma, and head and neck squamous cell cancer. HPV-seq detects cell-free HPV DNA across a large dynamic range and demonstrates accurate quantification even when few copies are present, enabling high-resolution molecular monitoring.
For the current study, the investigators conducted pre-clinical technical validation studies on HPV-seq and applied it retrospectively to a prospective multicenter cohort of locally-advanced cervix cancer patients and a cohort of oropharynx cancer patients. HPV-seq results were compared with those obtained by dPCR.
Results revealed that HPV-seq achieved reproducible detection of circulating HPV DNA at levels that were up to 20-fold lower than those detectable by dPCR. Detectable HPV ctDNA at end-of-treatment was associated with inferior progression free survival with 100% sensitivity and 67% specificity for recurrence. Accurate HPV genotyping was successful from 100% of the pre-treatment samples.
"Increasingly, as clinicians we are focused on precision medicine and making sure we are not over-treating people while still curing them. That is a very difficult balance to strike," said senior author Dr. Scott Bratman, assistant professor of radiation oncology and medical biophysics at Princess Margaret Cancer Centre. "We are really at the cusp of a revolution from a technology, clinical implementation, and standard of care standpoint, where five to 10 years from now we will not be treating everybody with the same dose of radiation and chemotherapy, and then waiting months to see if the treatment was effective. I am confident we will be giving much more tailored doses. Patients who need more treatment will then be able to continue on, or different treatments can be added. We can spare the vast majority of patients who will not need those interventions and provide them with a greater quality of life once they are cured of the cancer."
The HVP DNA bioassay paper was published in the September 27, 2021, online edition of the journal Clinical Cancer Research.
Related Links:
Princess Margaret Cancer Centre