Colorectal Cancer Relapse Predicted by ctDNA Clearance
By LabMedica International staff writers
Posted on 01 Jun 2021
Colorectal cancer (CRC) is the third most common cancer around the world with more than 1.9 million new cases diagnosed annually. CRC is also the second leading cause of cancer-related deaths with a 5-year mortality rate of about 40%.Posted on 01 Jun 2021
The existence of minimal residual disease (MRD), which is clinically occult and radiologically invisible at the time of surgery, has been considered the major source of disease recurrence. The direct and real-time measurement of MRD is an ideal solution to facilitate the decision-making in postsurgical management. Detection of circulating tumor DNA (ctDNA) holds great promise for this issue.
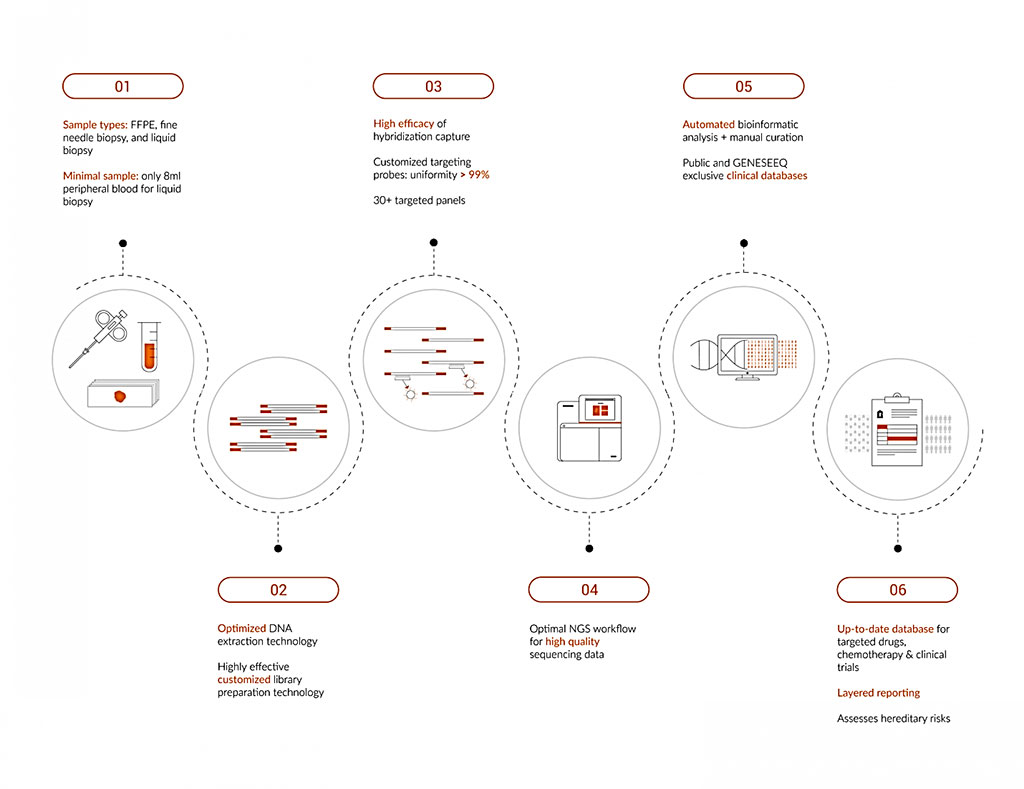
Image: Schematics of the workflow for the Geneseeq Prime 425-gene panel (Photo courtesy of Geneseeq Technology)
A team of Medical Oncologists at the Sun Yat-Sen University Cancer Center (Guangzhou, China) analyzed clinical and ctDNA data from 240 patients with stage II or stage III colorectal cancer who were recruited at three Chinese academic hospitals from 2017 to 2020. Tumor samples were collected at surgery, and blood samples were obtained seven days before surgery, within a week after surgery, six months after surgery, and every three months for the two years until patients passed away or withdrew study participation.
The peripheral blood leukocytes, primary tumors and plasma samples were all targeted-sequenced by the Geneseeq Prime 425-gene panel (Geneseeq Technology, Toronto, ON, Canada), yielding a mean sequencing depth of 276 ×, 1277 × and 4693 ×, respectively. All qualified variants identified in the primary tumor of each patient were regarded as patient-specific somatic variants for further ctDNA tracking. A plasma sample was declared as ctDNA-positive if the number of true variants detected in the plasma was more than 5% of the number of total tracking variants in each patient.
The scientists reported that in the first blood sample collected shortly after surgery, they found that 8.3% of patients were ctDNA positive, while 91.7% were ctDNA negative. Over the two-year follow-up, these ctDNA-negative patients were less likely than ctDNA-positive patients to have cancer recurrence, with a two-year recurrence-free survival rate of 89.4% versus 39.3%, respectively. Among the 20 ctDNA-positive patients, 60%, or 12 patients, experienced radiological relapse. Seven patients in this subset received adjuvant chemotherapy and became ctDNA negative, and one patient was lost to follow up.
Among the 17 ctDNA-positive patients who received adjuvant chemo, seven were recurrence-free at the two-year follow-up, while 10 still experienced recurrence. These findings suggested to the scientists that some patients who have remaining ctDNA can benefit from adjuvant chemo. Patients who were still ctDNA positive after adjuvant treatment had a 25% two-year recurrence-free survival rate compared to 87.7% for patients who were ctDNA negative after adjuvant chemotherapy. The patients who had remaining ctDNA after surgery and adjuvant chemotherapy were 12 times more likely to experience recurrence than patients who reached ctDNA-negative status.
The authors concluded that their large-scale, prospective, observational, and multicenter study suggests that serial detection of ctDNA could reflect the existence of MRD and identify disease recurrence ahead of radiological imaging. ctDNA evaluation, as early as 3–7 days postoperatively, may facilitate risk stratification and decision-making in the postsurgical management of patients with stage II/III CRC. The study was published on May 17, 2021 in the Journal of Hematology and Oncology.
Related Links:
Sun Yat-Sen University Cancer Center
Geneseeq Technology