Clonal Hematopoiesis of Indeterminate Potential Associated with hsC-Reactive Protein
By LabMedica International staff writers
Posted on 14 Jul 2020
Clonal hematopoiesis (CH) occurring in normally aging subjects, initially suggested by X-chromosome inactivation studies, is caused by acquired mutations in genes recurrently mutated in hematological cancers, and in non-driver candidates. Posted on 14 Jul 2020
Clonal hematopoiesis of indeterminate potential (CHIP) is predictive of hematological cancers and cardiovascular diseases, but the etiology of CHIP initiation and clonal expansion is unknown. Several lines of evidence suggest that proinflammatory cytokines may favor mutated hematopoietic stem cell expansion.
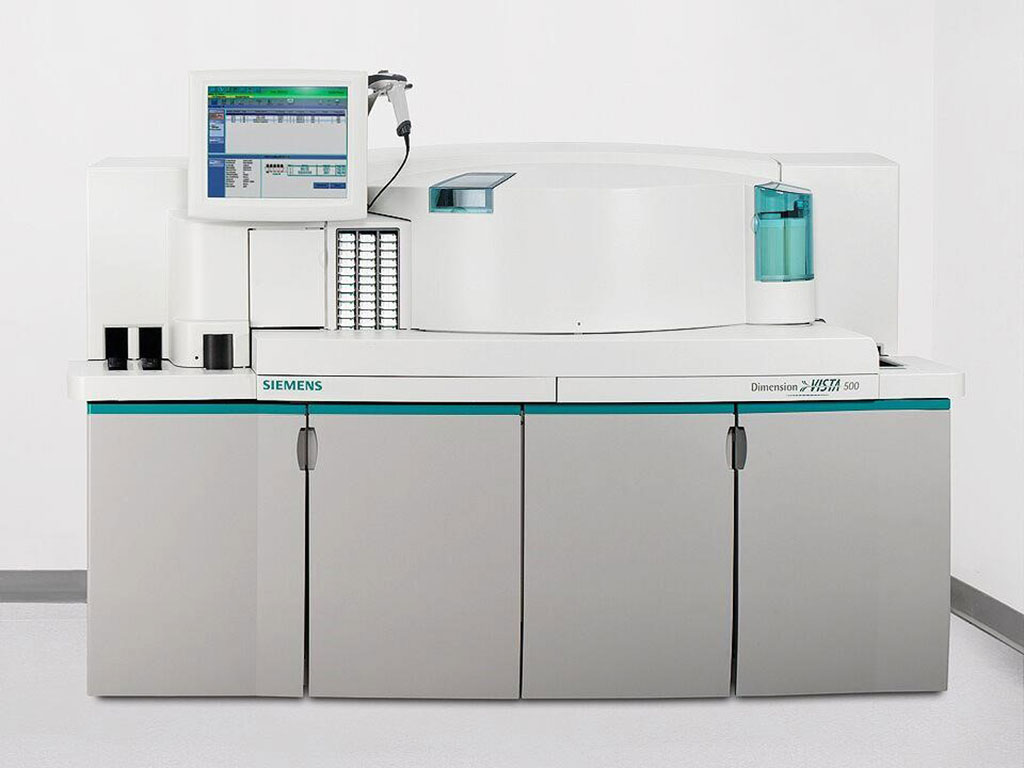
Image: The Dimension Vista 500 Intelligent Laboratory System (Photo courtesy of Siemens Healthineers).
A team of scientists at the Université de Montréal (Montreal, QC, Canada) and their associates investigated the potential link between inflammation and CHIP, and performed targeted deep sequencing of 11 genes previously implicated in CHIP in 1,887 subjects aged >70 years from the Montreal Heart Institute Biobank, of which 1,359 had prior coronary artery disease (CAD), and 528 controls did not.
The study subject’s DNA was sequenced at high coverage (95% >500×) on an Ion Proton sequencer using a custom Ampliseq “CHIP” panel (Thermo Fisher Scientific, Waltham, MA, USA) designed to target the top 11 genes reported in CHIP (ASXL1, CBL, DNMT3A, GNAS, GNB1, JAK2 [chr9:5073674- 5073808], PPM1D, SF3B1 [exons 14 to 16], SRSF2, TET2, and TP53) with 202 amplicons covering 38.49 kb. Highly Sensitive-C-reactive protein (hs-CRP) concentration was measured by quantitative immunonephelometric analysis on a Dimension Vista 500 Intelligent Laboratory System (Siemens Healthineers, Erlangen, Germany) and hs-CRP is a validated biomarker of inflammation.
The scientists identified CHIP in 427 of the 1,887 subjects (22.6%). CHIP mutations were more frequently identified in DNMT3A (11.6%) and TET2 (6.1%), with a higher proportion of TET2 mutations occurring in controls than in patients with CAD (9.0% versus 4.9%). Mutations in DNMT3A, TET2, and ASXL1 accounted for the majority of mutations (82.9%). CHIP carriers had 21% higher hs-CRP levels compared with their non-carrier counterparts (median: 1.60 mg/L versus 1.41 mg/L) and a similar effect was observed in the subgroup of patients with known CAD.
The authors concluded that their study highlights the role of inflammation in CHIP. The etiology of CHIP is probably multifactorial, and several other factors need to be identified. Clinical trials should test whether anti-inflammatory therapy can reduce CHIP progression and related diseases. The study was published on June 3, 2020 in the journal Blood Advances.














