Precision Medicine-Based Genetic Testing Developed for Prostate Cancer
By LabMedica International staff writers
Posted on 01 Jul 2020
Germline testing (GT) is a central feature of prostate cancer (PCA) treatment, management, and hereditary cancer assessment. Critical needs include optimized multigene testing strategies that incorporate evolving genetic data, consistency in GT indications and management, and alternate genetic evaluation models that address the rising demand for genetic services.Posted on 01 Jul 2020
As PCA GT has increased, new practice and implementation challenges have emerged in three major areas: expanded options for multigene panels, with a resultant lack of clarity regarding optimized panel use and priority genes to test; variability in guidelines regarding GT indications and genetically based management that incorporates emerging data; and a shortage of genetic services.
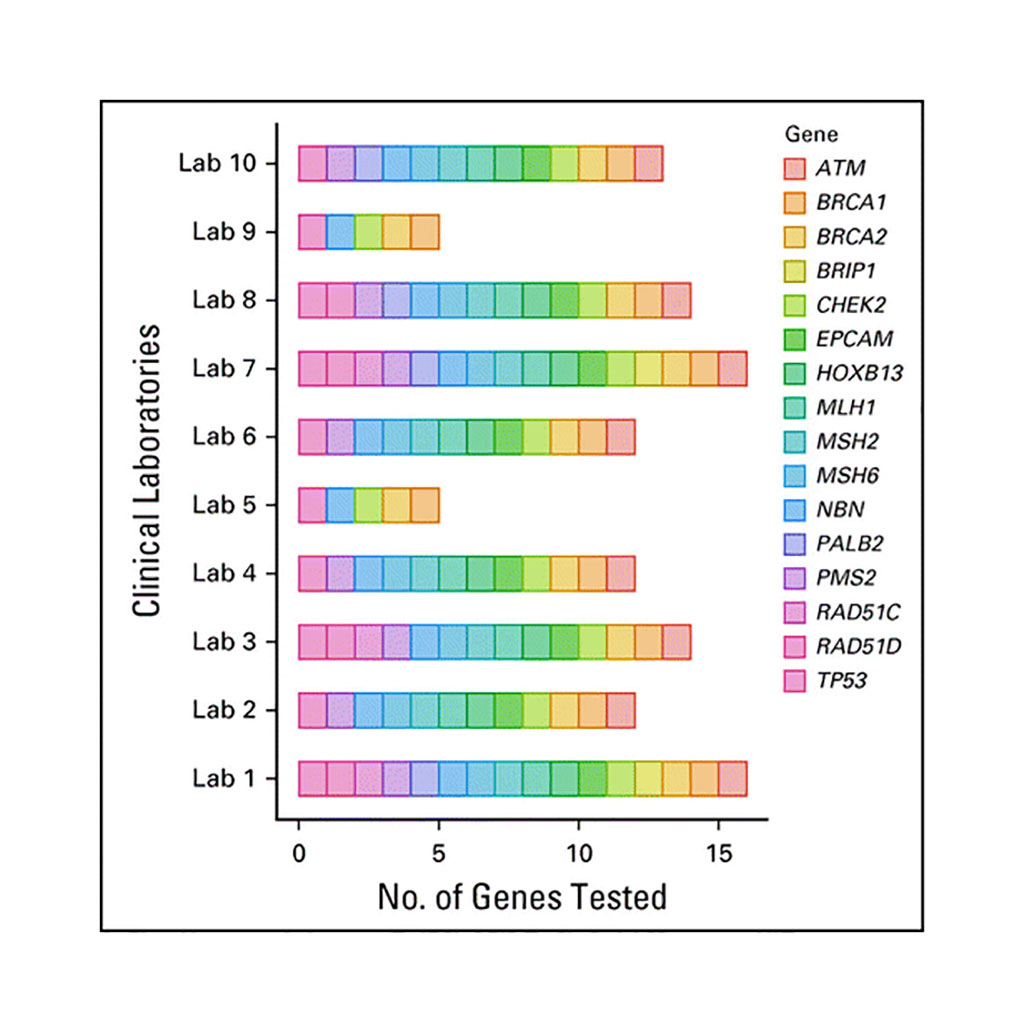
Image: Variability in prostate cancer–specific multigene panels; genetic testing registry as of August 2019 (Photo courtesy of Saud H. AlDubayan, MD).
An international panel of cancer scientists led by the Thomas Jefferson University (Philadelphia, PA, USA) have developed a multidisciplinary, consensus-driven framework for genetic testing of prostate cancer patients. The overarching questions they sought to address were the primary drivers of the conceptual framework: Which men should be considered for germline prostate cancer genetic testing? Which panels should be considered and which genes should be prioritized for testing? What prostate cancer-specific recommendations should be considered on the basis of genetic results? What is optimal informed consent for prostate cancer germline testing? What collaborative strategies may facilitate prostate cancer genetic evaluation between healthcare and genetic providers? What post-test disclosure strategies are most appropriate on the basis of genetic results? What barriers must be addressed to enhance prostate cancer germline testing?
The panel recommended large germline panels and somatic testing for metastatic prostate cancer. They also recommended germline testing for metastatic disease or family history suggestive of hereditary prostate cancer. Additional family history and pathologic criteria garnered moderate consensus. Priority genes to test for metastatic disease treatment included BRCA2, BRCA1, and mismatch repair genes, with broader testing, such as ATM, for clinical trial eligibility. The panel recommended BRCA2 for active surveillance discussions, while screening starting at age 40 years or 10 years before the youngest prostate cancer diagnosis in a family was recommended for BRCA2 carriers, with consideration in HOXB13, BRCA1, ATM, and mismatch repair carriers.
The panel also developed point-of-care evaluation models for healthcare and genetic providers to work collaboratively to address the genetic counseling shortage. The genetic evaluation framework included optimal pretest informed consent, post-test discussion, cascade testing, and technology-based approaches.
Veda N. Giri, MD, an Associate Professor in Medical Oncology and first author of the study, said, “Germline mutations are found in 12% to 17% of men with metastatic prostate cancer and 7% of men with early-stage disease. A patient's genetic information may inform how healthcare providers screen, diagnose, and treat prostate cancer, as well as enable them to enroll in a clinical trial. Therefore, this implementation framework applies to oncologists, urologists, genetic counselors, and primary care providers engaged in the care of men with prostate cancer or at risk for the disease.” The study was published on June 9, 2020 in the Journal of Clinical Oncology.
Related Links:
Thomas Jefferson University








 Analyzer.jpg)