MicroRNA Biomarker Panel Identifies Patients at Risk for Pancreatic Cancer Metastasis to the Lymph Nodes
By LabMedica International staff writers
Posted on 26 May 2020
A team of cancer researchers has identified a microRNA (miRNA) signature panel that identifies patients at risk for pancreatic cancer metastasis to the lymph nodes. Posted on 26 May 2020
There are usually no early symptoms for pancreatic cancer, and symptoms that are specific enough to suggest presence of the disease typically do not develop until it has reached an advanced stage. By this time pancreatic ductal adenocarcinomas (PDACs) frequently have metastasized to the lymph nodes. Therefore, strategies are needed to identify patients at highest risk for lymph node metastases.
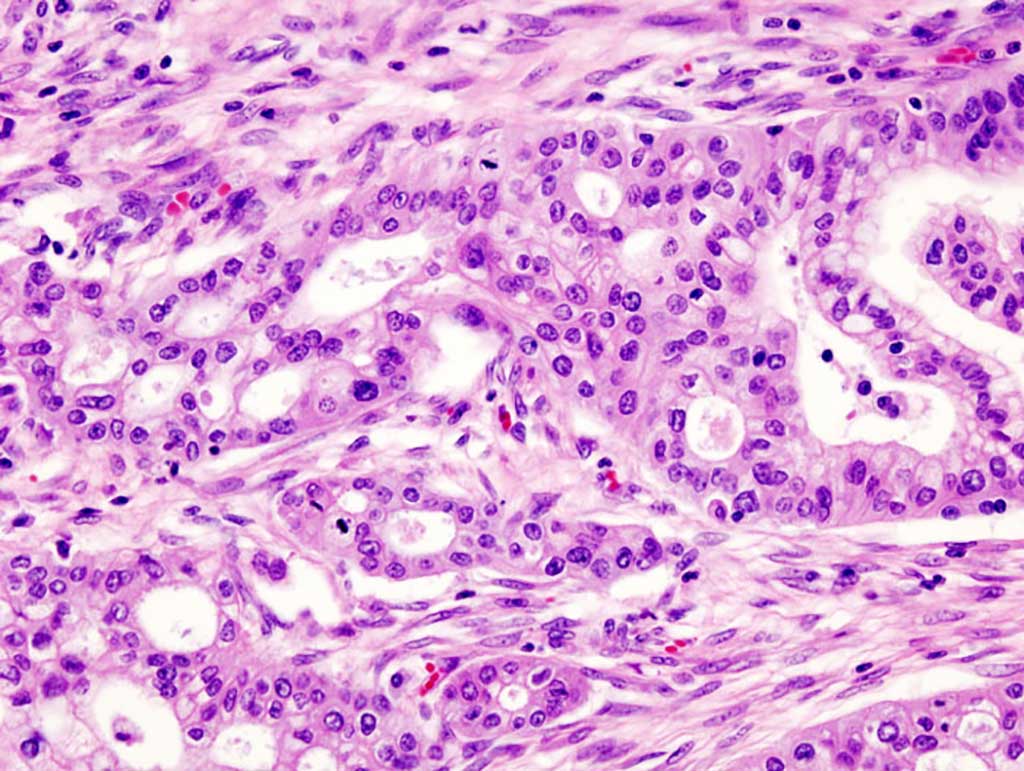
Image: Micrograph of pancreatic ductal adenocarcinoma (the most common type of pancreatic cancer) (Photo courtesy of Wikimedia Commons)
In this regard, investigators at the Beckman Research Institute of City of Hope Comprehensive Cancer Center, Duarte (CA, USA) performed genome-wide expression profile analyses of PDAC specimens, collected during surgery or endoscopic ultrasound fine-need aspiration (EUS-FNA), to identify a microRNA (miRNA) signature associated with metastasis to lymph nodes.
MicroRNAs (miRNAs) comprise a class of about 20 nucleotides-long RNA fragments that block gene expression by attaching to molecules of messenger RNA in a fashion that prevents them from transmitting the protein synthesizing instructions they had received from the DNA. With their capacity to fine-tune protein expression via sequence-specific interactions, miRNAs help regulate cell maintenance and differentiation. In addition to miRNAs playing an essential role in tumor development, dysregulation of certain miRNAs has been associated with many different diseases, such as dementia, and cardiovascular conditions.
For this study, the investigators analyzed miRNA expression profiles of primary pancreatic tumors from three public datasets. They then analyzed 157 PDAC specimens (83 from patients with lymph node metastases and 74 without) from Japan, collected from 2001 through 2017, for the training cohort and a 107 PDAC specimens (63 from patients with lymph node metastases and 44 without) from a different medical center in Japan, from 2002 through 2016, for the validation cohort.
The investigators also analyzed samples collected by EUS-FNA before surgery from 47 patients (22 patients with lymph node metastases and 25 without; 17 for the training cohort and 30 from the validation cohort), and 62 specimens prior to any treatment from patients who received neoadjuvant chemotherapy (nine patients with lymph node metastasis and 53 without) for additional validation. The median follow-up was 5.5 years in the testing or training cohort and 2.8 years for the validation cohort.
Results revealed a miRNA expression pattern associated with diagnosis of PDAC metastasis to lymph nodes. The panel comprised six miRNAs: miR-155-5p, miR-196b-5p, miR-365a-5p, miR-629-5p, miR-675-3p, and miR-92b-3p. This panel discriminated patients with vs without lymph node metastases with an area under the curve (AUC) of 0.84. In the validation cohort, the panel identified patients with vs without lymph node metastases with an AUC of 0.73. In EUS-FNA biopsies, the model identified patients with vs without lymph node metastases with an AUC of 0.78.
"This may not seem like a high percentage but in a clinical setting, especially when we do not currently have a pancreatic cancer screening tool, this accuracy level has few equals," said senior author Dr. Ajay Goel, chairman of the department of molecular diagnostics and experimental therapeutics at the Beckman Research Institute of City of Hope Comprehensive Cancer Center. "If we know beforehand that these pancreatic cancer patients have lymph node metastases, we probably would not perform surgery because it is complicated, expensive and, most importantly, patients with lymph node spread do not do well after surgery. Instead, we would likely first treat the patient with chemotherapy to kill all the loose-hanging cells in the lymph nodes and then surgically remove the cancer from the pancreas."
The pancreatic cancer metastasis study was published in the May 3, 2020, online edition of the journal Gastroenterology.
Related Links:
Beckman Research Institute of City of Hope Comprehensive Cancer Center













