New Risk Loci Identified for Polycystic Ovary Syndrome
By LabMedica International staff writers
Posted on 09 Jan 2019
Polycystic ovary syndrome is a disorder characterized by hyperandrogenism, ovulatory dysfunction and polycystic ovarian morphology. Affected women frequently have metabolic disturbances including insulin resistance and dysregulation of glucose homeostasis.Posted on 09 Jan 2019
Polycystic ovary syndrome (PCOS) is diagnosed with two different sets of diagnostic criteria, resulting in a phenotypic spectrum of PCOS cases. The genetic similarities between cases diagnosed based on the two criteria have been largely unknown.
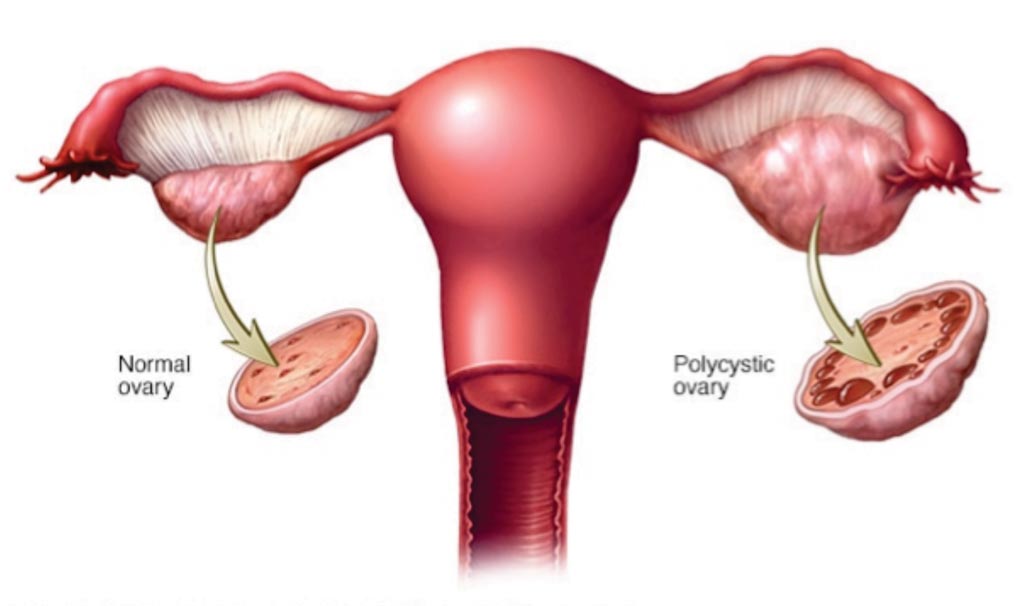
Image: A diagram showing normal and polycystic ovary syndrome, in the latter the ovaries may develop numerous small collections of fluid (follicles) and fail to regularly release eggs (Photo courtesy of Mayo Clinic).
An international team of scientists working with the University of Utah (Salt Lake City, UT) performed a genome-wide association study meta-analysis involving 10,074 individuals with PCOS and 103,164 without, leading to three previously undetected loci and 11 loci linked to the endocrine disorder in the past. Of those, 13 loci were associated with self-reported PCOS and cases diagnosed using National Institutes of Health or Rotterdam criteria.
PCOS diagnoses are based on excess androgen hormone levels and ovulatory dysfunction, the team explained, which represents roughly 7% of reproductive age women around the world. On the other hand, more general criteria from Rotterdam defined PCOS as polycystic ovarian morphology in combination with either hyperandrogenism or ovulatory dysfunction, representing an estimated 15% to 20% of women globally.
The team reported new associations at loci in or around the PLGRKT, ZBTB16, and MAPRE1 genes, which are believed to contribute to metabolic and reproductive pathways. The meta-analysis also led to 11 known risk loci, which were overrepresented for variants in and around genes from neuroendocrine and metabolic pathways. The set of known risk loci included half a dozen sites previously implicated in PCOS in women of Han Chinese ancestry, and a variant near the GATA4/NEIL2 genes that showed strong ties to the PCOS diagnosed using NIH criteria but weaker associations to the self-reported PCOS cases.
The authors concluded that the genetic underpinnings of PCOS implicate neuroendocrine, metabolic, and reproductive pathways in the pathogenesis of disease. Although specific phenotype stratified analyses are needed, genetic findings were consistent across the diagnostic criteria for all but one susceptibility locus, suggesting a common genetic architecture underlying the different phenotypes. The study was published on December 19, 2018, in the journal PLOS Genetics.
Related Links:
University of Utah














