Genetic Connections Uncovered Between Psychiatric Disorders
By LabMedica International staff writers
Posted on 12 Jul 2018
Brain disorders may exhibit shared symptoms and substantial epidemiological comorbidity, inciting debate about their etiologic overlap. However, detailed study of phenotypes with different ages of onset, severity, and presentation poses a considerable challenge.Posted on 12 Jul 2018
Over the past century, the classification of brain disorders has evolved to reflect the medical and scientific communities’ assessments of the presumed root causes of clinical phenomena such as behavioral change, loss of motor function, or alterations of consciousness. Psychiatric disorders share a genetic overlap with each other that neurological disorders do not.
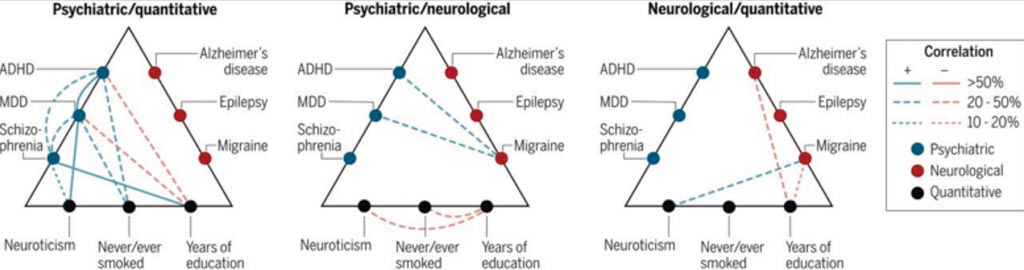
Image: Genetic risk correlations among brain disorders and quantitative phenotypes (Photo courtesy of the Brainstorm Consortium).
A large team of scientists led by those at Massachusetts General Hospital (Boston, MA, USA) quantified the genetic sharing of 25 brain disorders from genome-wide association studies of 265,218 patients and 784,643 control participants and assessed their relationship to 17 phenotypes from 1,191,588 individuals. The team used a linkage disequilibrium score regression approach they developed to calculate heritability estimates and correlations.
The scientists found that common variant risk for psychiatric disorders was shown to correlate significantly, especially among attention deficit hyperactivity disorder (ADHD), bipolar disorder, major depressive disorder (MDD), and schizophrenia. By contrast, neurological disorders appear more distinct from one another and from the psychiatric disorders, except for migraine, which was significantly correlated to ADHD, MDD, and Tourette syndrome. In the general population, the personality trait neuroticism is significantly correlated with almost every psychiatric disorder and migraine. Schizophrenia correlated with many psychiatric disorders, whereas the immunopathological affliction Crohn's disease did not, and posttraumatic stress syndrome was also largely independent of underlying traits. Essentially, the earlier the onset of a disorder, the more inheritable it appeared to be.
Ben Neale, PhD, an associate professor and co-lead author of the study, said, “This work is starting to reshape how we think about disorders of the brain. If we can uncover the genetic influences and patterns of overlap between different disorders, then we might be able to better understand the root causes of these conditions, and potentially identify specific mechanisms appropriate for tailored treatments.”
The author concluded that the high degree of genetic correlation among many of the psychiatric disorders adds further evidence that their current clinical boundaries do not reflect distinct underlying pathogenic processes, at least on the genetic level. The study was published on June 22, 2018, in the journal Science.
Related Links:
Massachusetts General Hospital














