Esophageal Cancer GWAS Leads to Risk Variants
By LabMedica International staff writers
Posted on 16 Feb 2018
Genome-wide association studies have identified common variants associated with risk of esophageal squamous cell carcinoma; however, these common variants cannot explain all heritability of esophageal cancer.Posted on 16 Feb 2018
New germline contributors to esophageal squamous cell carcinoma (ESCC) risk have been revealed, including a low-frequency change to the Cytochrome P450 Family 26 Subfamily B Member 1, (CYP26B1) drug metabolism gene that appears to affect blood serum levels of a tumor suppressor called all-trans retinoic acid (atRA).
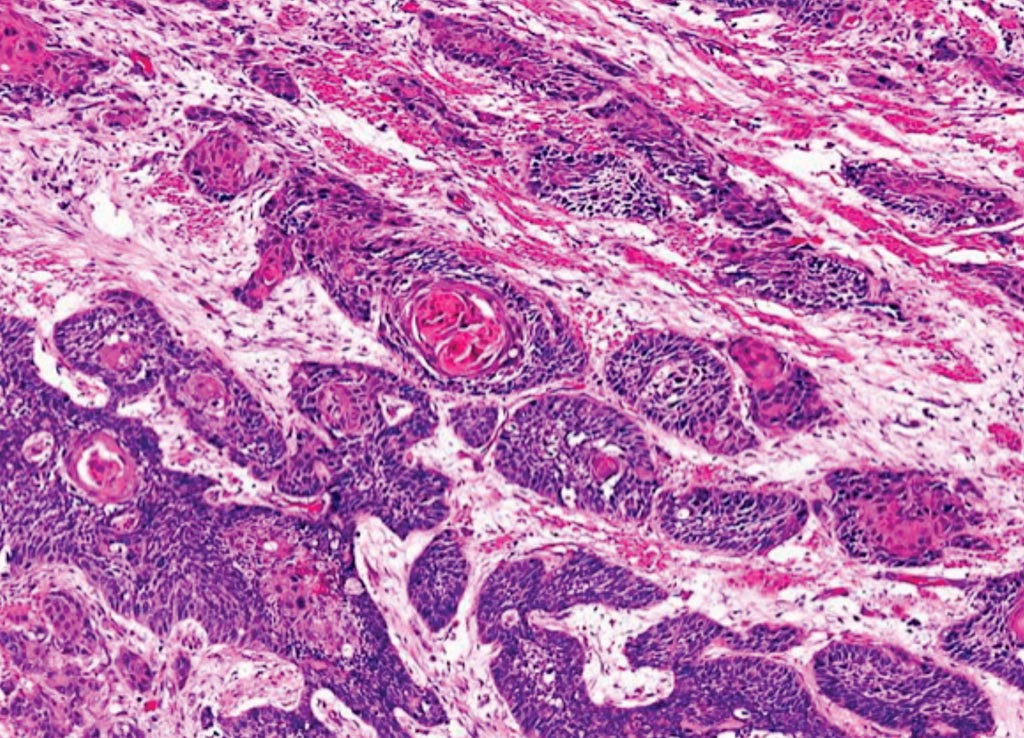
Image: A histopathology of esophageal squamous cell carcinoma with keratin pearl formation (Photo courtesy of Dr. Dharam Ramnani, MD).
Scientists at the Chinese Academy of Medical Sciences (Beijing, China) and their colleagues used exome sequences for more than 3,700 individuals with ESCC and nearly 3,900 individuals without. They looked for single-nucleotide polymorphisms (SNPs) or low-frequency variants associated with risk of the disease, which is especially common in parts of China. From these data, they narrowed in on half a dozen risk sites that could be replicated in another 7,002 cases and 8,757 controls, including three common SNPs and three low-frequency variants.
The team used Illumina HumanExome BeadChip arrays to profile low-frequency protein-coding variants in the ESCC cases and the controls from Beijing. After excluding samples with insufficient or low-quality data, they were left comparing exome patterns for 3,714 of the ESCC cases and 3,880 controls, an analysis that led to 30 suspicious variants. The team attempted to verify the potential ESCC risk variants with OpenArray- or TaqMan-based genotyping on individuals from two replication cohorts: 3,120 ESCC cases and 3,919 controls from Wuhan province and another 3,882 individuals with ESCC and 4,838 without from the Chinese province of Hebei.
The scientists uncovered six new risk variants at four sites in or around the CCHCR1, TCN2, TNXB, LTA, CYP26B1, and FASN genes. Three of the associations at the TCN2, CYP26B1, and FASN gene loci, were based on low-frequency variants that appeared to have higher-than-usual effect sizes. An ESCC-associated variant at CYP26B1, called rs138478634, had particularly close ties to ESCC risk in individuals with a history of smoking and/or drinking, although the team noted that rs138478634 was not linked to smoking or drinking status in control individuals. Through a series of follow-up cell line and patient serum expression profiling experiments, the group saw lower-than-usual levels of the atRA tumor suppressor in cells or individuals pumping out the rs138478634 variant-containing version of CYP26B1.
The authors concluded that results of the new study extended previous findings and advanced our understanding of the genetic etiology of ESCC, which might be useful for risk assessment, early detection, and targeted treatment of ESCC. The study was published on January 29, 2018, in the journal Nature Genetics.
Related Links:
Chinese Academy of Medical Sciences













