Prion Protein Found in Skin of CJD Patients
By LabMedica International staff writers
Posted on 07 Dec 2017
Creutzfeldt-Jakob disease (CJD) is an incurable, and ultimately fatal, transmissible, neurodegenerative disorder in the family of prion diseases. Prion diseases originate when normally harmless prion protein molecules become abnormal and gather in clusters and filaments in the human body and brain.Posted on 07 Dec 2017
Most people associate prion diseases with the brain, although scientists have found abnormal infectious prion protein in other organs, including the spleen, kidney, lungs and liver. Sporadic CJD (sCJC) is known to be transmissible by invasive medical procedures involving the central nervous system and cornea, but transmission via skin had not been a common concern.
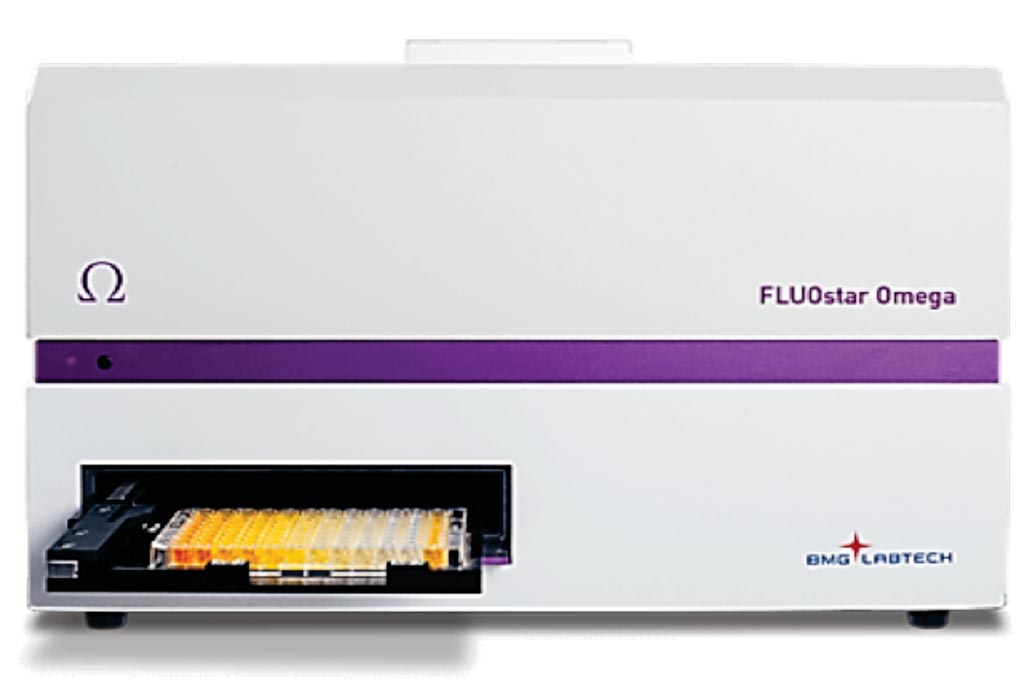
Image: The FLUOstar Omega multi-mode microplate reader. A newly developed prion seeding assay called Real-Time Quaking Induced Conversion assay (RT-QuIC), scientists can now measure prion seeding at lower levels and in less than a few days in standard 96-well microplates (Photo courtesy of BMG Labtech).
A large team of scientists working with the National Institutes of Health’s Rocky Mountain Laboratories (Hamilton, MT. USA) explored the potential prion seeding activity and infectivity of skin from sCJD patients. Autopsy or biopsy skin samples from 38 patients (21 sCJD, two variant CJD (vCJD), and 15 non-CJD) were analyzed by Western blotting and real-time quaking-induced conversion (RT-QuIC) for PrPSc. Skin samples from two patients were further examined for prion infectivity by bioassay using two lines of humanized transgenic mice.
The tem reported that Western blotting revealed dermal PrPSc in one of five deceased sCJD patients and one of two vCJD patients. However, the more sensitive RT-QuIC assay detected prion seeding activity in skin from all 23 CJD decedents, but not in skin from any non-CJD control individuals (with other neurological conditions or other diseases) during blinded testing. Although sCJD patient skin contained ~103- to 105-fold lower prion seeding activity than did sCJD patient brain tissue, all 12 mice from two transgenic mouse lines inoculated with sCJD skin homogenates from two sCJD patients succumbed to prion disease within 564 days after inoculation.
Byron Caughey, PhD, a senior investigator who helped oversee the study said, “Our objective has always been to facilitate RT-QuIC testing using the most broadly available and least-invasive sample possible, whether that is blood, skin, nasal brushings, or other samples. This study used humanized mice with tissue extracts directly inoculated into the brain, so the system was highly primed for infection. There is no evidence that transmission can occur in real-world situations via casual skin contact.” The study was published on November 22, 2017, in the journal Science Translational Medicine.
Related Links:
National Institutes of Health Rocky Mountain Laboratories













