HLF-Gene Controls Generation of Immune System
By LabMedica International staff writers
Posted on 06 Dec 2017
Blood stem cells give rise to all of the blood cells, the red blood cells that transport oxygen, the platelets that enable blood coagulation, and our immune cells that protect us from infections.Posted on 06 Dec 2017
Immune cells can, in turn, be divided into two groups; one that consists of cells with a very short life expectancy and a natural but rather unspecific ability to counteract infections (myeloid cells), and another that, in contrast, consists of very long-lived cells (lymphocytes) that specialize in combatting specific bacteria and viruses.
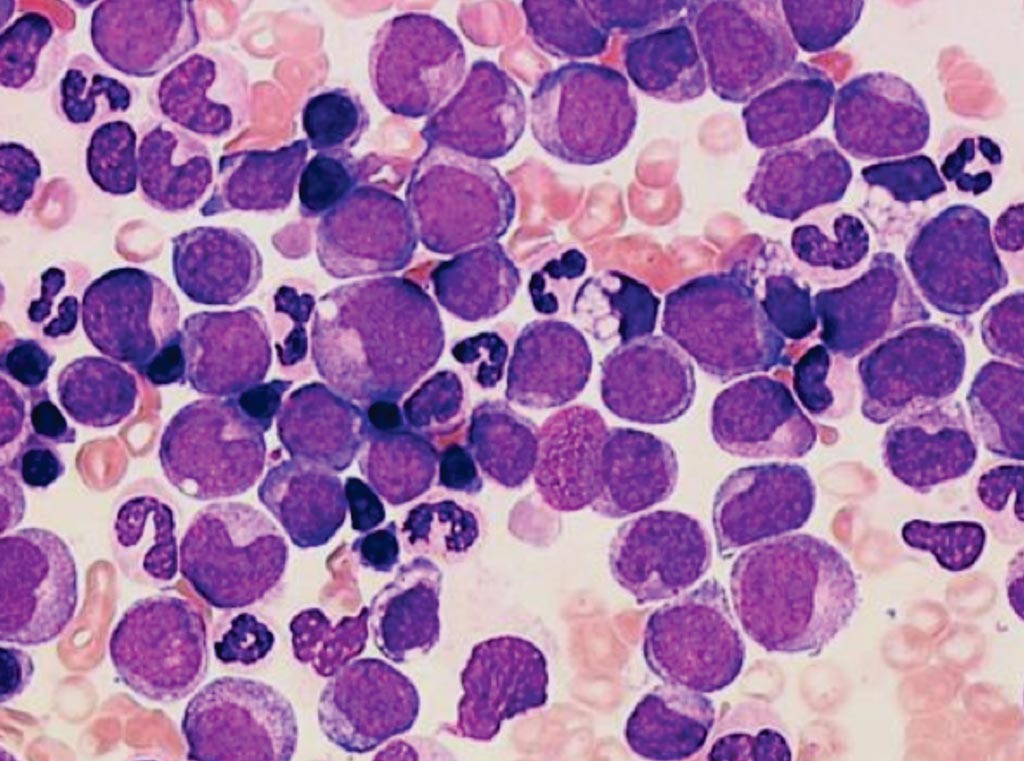
Image: A bone marrow aspirate from a patient with acute myeloid leukemia (Photo courtesy of Cytogenetic Oncology Laboratory).
An international team of scientists collaborating with Lund University (Lund, Sweden) personnel identified robust expression of the leukemia-associated transcription factor hepatic leukemia factor (Hlf) in normal multipotent hematopoietic progenitors, which was rapidly downregulated upon differentiation. Interference with its normal downregulation revealed Hlf as a strong negative regulator of lymphoid development, while remaining compatible with myeloid fates.
They also observed rapid lymphoid commitment upon reduced Hlf activity. The arising phenotypes resulted from Hlf binding to active enhancers of myeloid-competent cells, transcriptional induction of myeloid, and ablation of lymphoid gene programs, with Hlf induction of nuclear factor I C (Nfic) as a functionally relevant target gene. Patients with leukemia in which the HLF gene is involved have a very poor prognosis, but it has been difficult to generate reliable models for studying the emergence, development and possible treatment of these leukemias more thoroughly.
David Bryder, PhD, a professor and lead investigator of the study, said, “Our studies revealed that if the immature blood cells are unable to shut down the HLF gene at the correct stage of development, the lymphocytes, the long-lived immune cells, are unable to form. As a result, you will only have one type of immune defense. An increased understanding of these processes is crucial as immune cells in patients who undergo bone marrow transplants are regenerated very slowly, which results in a long period of immune sensitivity.” The study was published on November 21, 2017, in the journal Cell Reports.
Related Links:
Lund University











 (3) (1).png)