Type 2 Diabetes Misdiagnosed in African Americans
By LabMedica International staff writers
Posted on 27 Sep 2017
Glycated hemoglobin (HbA1c) is used to diagnose type 2 diabetes (T2D) and assess glycemic control in patients with diabetes. Previous genome-wide association studies (GWAS) have identified 18 HbA1c-associated genetic variants.Posted on 27 Sep 2017
One genetic variant in particular, found only in African Americans, significantly reduces the accuracy of the HbA1c blood test used to diagnose and monitor the condition. This means around 650,000 African Americans in the USA could have undiagnosed type 2 diabetes if tested with the HbA1c test alone.

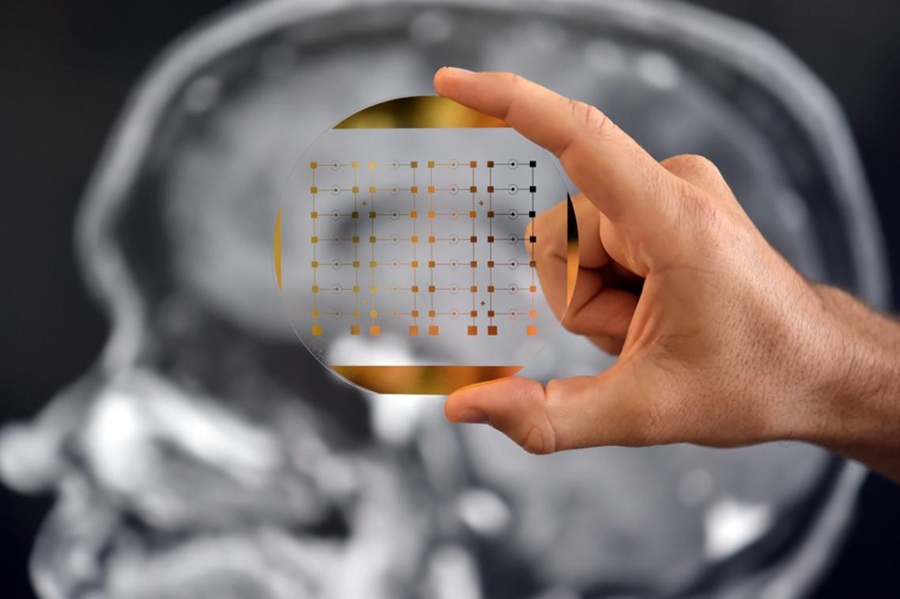
Image: The Affymetrix Genome-Wide Human SNP Array 6.0 features 1.8 million genetic markers including more than 906,600 single nucleotide polymorphisms (SNPs) and more than 946,000 probes for the detection of copy number variation (Photo courtesy of Thermo Fisher Scientific).
A large team of 200 international scientists led by those at the Welcome Trust Sanger Institute (Hinxton, Cambridge, UK) used genome-wide association meta-analyses in up to 159,940 individuals from 82 cohorts of European, African, East Asian, and South Asian ancestry. They identified 60 common genetic variants associated with HbA1c. They classified variants as implicated in glycemic, erythrocytic, or unclassified biology and tested whether additive genetic scores of erythrocytic variants (GS-E) or glycemic variants (GS-G) were associated with higher T2D incidence in multiethnic longitudinal cohorts.
Each cohort was genotyped on commercially available genome-wide arrays, for instance, the Affymetrix Genome-Wide Human SNP Assay 6.0 or the Illumina Human610-Quad BeadChip) or the Illumina CardioMetabochip (Metabochip). Where possible, studies reported HbA1c as a National Glycohemoglobin Standardization Program (NGSP) percent. All participants were free of diabetes defined by physician diagnosis, medication use, or fasting glucose (FG) ≥ 7 mmol/L. A small number of cohorts also removed individuals with two hour glucose (2hrGlu) ≥ 11.1 mmol/L, or HbA1c ≥ 6.5%.
The teams found that 19 glycemic and 22 erythrocytic variants were associated with HbA1c at genome-wide significance. GS-G was associated with higher T2D risk, whereas GS-E was not. In Europeans and Asians, erythrocytic variants in aggregate had only modest effects on the diagnostic accuracy of HbA1c. Yet, in African Americans, the X-linked Glucose-6-phosphate dehydrogenase (G6PD) G202A variant (T-allele frequency 11%) was associated with an absolute decrease in HbA1c of 0.81%-units per allele in hemizygous men, and 0.68%-units in homozygous women.
Inés Barroso, PhD, a principal investigator and a senior author of the study said, “The issue with the G6PD genetic variant is it artificially lowers the value of blood sugar in the HbA1c test, and can lead to under-diagnosis of people with type 2 diabetes. We estimate that if we tested all Americans for diabetes using the HbA1c test, we would miss type 2 diabetes in around 650,000 African Americans. However, the HbA1c test remains a suitable test for diagnosing and monitoring diabetes for the majority of people.” The study was published on September 12, 2017, in the journal Public Library of Science Medicine.
Related Links:
Welcome Trust Sanger Institute