Test Discriminates Between Viral and Bacterial Infections
By LabMedica International staff writers
Posted on 10 Aug 2017
Lower respiratory tract infection (LRTI) commonly causes hospitalization in adults but because bacterial diagnostic tests are not accurate, antibiotics are frequently prescribed. Antibiotics are lifesaving drugs, but overuse is leading to antibiotic resistance, one of the world's most pressing health threats.Posted on 10 Aug 2017
Although sensitive molecular diagnostics such as polymerase chain reaction (PCR) allow clinicians to rapidly and accurately diagnose a wide variety of respiratory viruses, their impact on management and antibiotic prescription has been modest primarily due to concern about bacterial co-infection.
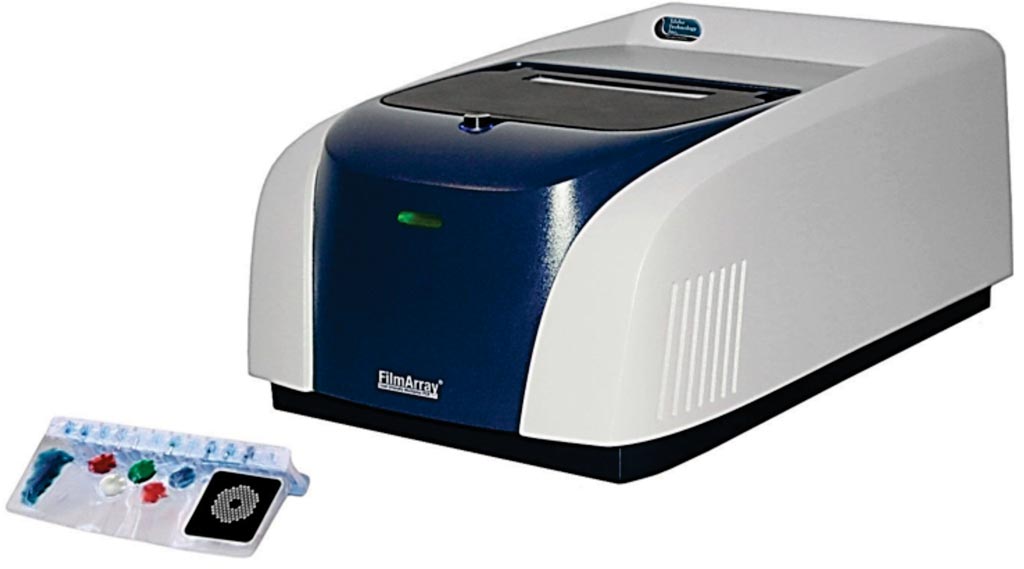
Image: The FilmArray respiratory panel enables rapid and accurate automated detection of pathogens causing respiratory infections (Photo courtesy of Idaho Technologies).
Scientists at the University of Rochester School of Medicine (Rochester, NY, USA) recruited a group of 94 adults hospitalized with lower respiratory tract infections. The team gathered clinical data, took blood from each patient, and conducted a battery of microbiologic tests to determine which of 41 patients had a bacterial infection and which of 53 patients had a non-bacterial or viral infection. Patients were enrolled within 24 hours of admission and demographic, clinical and laboratory information collected.
Nose and throat swabs (NTS), sputum, urine, and blood samples obtained at admission for bacterial and viral detection were processed at the hospital’s clinical laboratories. Urine was assayed for Streptococcus pneumoniae antigen using Binax NOW. NTS and sputum were tested using the real time multiplex PCR for detection of 15 viruses and three atypical bacteria. For RNAseq, cDNA libraries were generated using 200 ng of globin-reduced total RNA from each sample. Libraries were sequenced (single end reads) on the Illumina HiSeq 2500.
The investigators showed that RNAseq and qPCR confirmed significant differences in mean expression for 10 genes previously identified as discriminatory for bacterial LRTI. A novel dimension reduction strategy selected three pathways (lymphocyte, α-linoleic acid metabolism, IGF regulation) including eleven genes as optimal markers for discriminating bacterial infection. Using these genes, they constructed a classifier for bacterial LRTI with 90% (79% CV) sensitivity and 83% (76% CV) specificity. This novel, pathway-based gene set displays promise as a method to distinguish bacterial from nonbacterial LRTI.
Ann R. Falsey, MD, a professor and the lead study author, said, “It's extremely difficult to interpret what's causing a respiratory tract infection, especially in very ill patients who come to the hospital with a high fever, cough, shortness of breath and other concerning symptoms. My goal is to develop a tool that physicians can use to rule out a bacterial infection with enough certainty that they are comfortable, and their patients are comfortable, foregoing an antibiotic.” The study was published on July 26, 2017, in the journal Scientific Reports.
Related Links:
University of Rochester School of Medicine














