Rapid Molecular Testing Enables Faster, More Targeted Antibiotic Treatment for Pneumonia
Posted on 12 Mar 2024
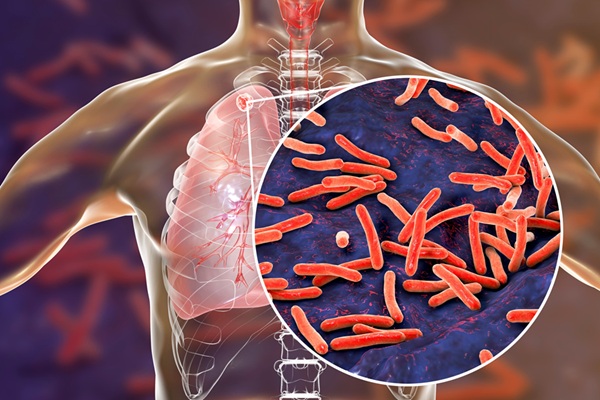
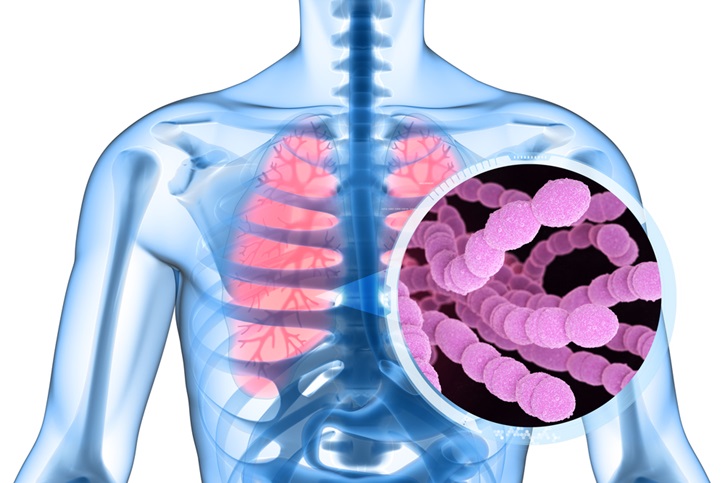
Pneumonia, an inflammation of the lungs typically caused by viral or bacterial infection, is a leading infectious disease worldwide, contributing significantly to global mortality and morbidity. Community-acquired pneumonia (CAP) refers to pneumonia contracted outside healthcare settings. While culture-based methods have been the norm for diagnosing bacterial pneumonia, these often detect pathogens only 20% to 40% of the time and yield slower results, hindering early, precise antibiotic therapy. Now, a randomized controlled trial (RCT) has demonstrated that utilizing rapid molecular testing in emergency departments (ED) can lead to more accurately targeted antibiotic treatment for pneumonia.
In the trial conducted at Haukeland University Hospital (HUS, Bergen, Norway), adult patients presenting with CAP symptoms in the ED were randomly divided into two groups. One group received rapid syndromic polymerase chain reaction (PCR) testing with the BioFire FilmArray Pneumonia plus panel (FAP plus), which identifies 27 bacterial and viral respiratory pathogens. The other group underwent standard microbiologic testing methods including blood culture, pneumococcal urine test, and an in-house PCR test. The main goals were to assess the delivery of pathogen-specific treatment based on test results and the timeframe for providing such treatment within 48 hours of randomization. Pathogen-specific treatment was categorized as a change, continuation, or discontinuation of antibiotic treatment depending on the results.
The results showed that patients who underwent rapid syndromic PCR testing were more likely to receive pathogen-specific antibiotic treatments compared to those who had standard microbiologic testing. Additionally, they received appropriate treatment more quickly. These findings suggest that rapid syndromic PCR tests could potentially enhance or even replace traditional culture-based diagnostic methods for lower respiratory infections. While the trial was limited to a single hospital setting and had a small sample size, the researchers believe the results are applicable to similar hospital environments.
"We sought to reduce the time to provision of pathogen-directed treatment, potentially decreasing unnecessary or broad-spectrum antibiotic use and fostering antimicrobial stewardship," stated the researchers. "Future research should continue to explore innovative approaches to improving the diagnosis and management of respiratory infections, such as incorporating clinical decision support tools and antimicrobial stewardship programs into routine practice."
Related Links:
HUS