Microbial Sensor Identifies Bacterial Infections and Also Creates Blood Stem Cells
Posted on 26 Dec 2023
A new study has revealed that a microbial sensor, known as Nod1, crucial in detecting and combating bacterial infections, also significantly influences the formation of blood stem cells. This discovery could revolutionize the process of generating patient-specific blood stem cells, potentially eliminating the need for bone marrow transplants. Previous research indicated that while inflammatory signals typically trigger immune responses, they serve a different purpose during the early stages of embryonic development, particularly in the formation of vascular systems and blood. The activation of the microbial sensor in embryos prompts the transformation of vascular endothelial cells into blood stem cells, creating the potential for the development of a new method to replicate this process in a laboratory setting using a patient's own blood.
Stem cells are critical for the body's development and repair, continuously dividing to maintain their population and generate specialized cells. Embryonic pluripotent stem cells have the capability to form any cell type required by the body, while adult stem cells are more specialized. Hematopoietic stem cells, or blood stem cells, are responsible for producing all the components of blood. These essential cells are formed before birth within the embryo. Researchers at Iowa State University (Ames, IA, USA) discovered that the immune receptor Nod1 activates in an embryo before endothelial cells begin their transition into becoming stem cells, essentially preparing them for this transformation.
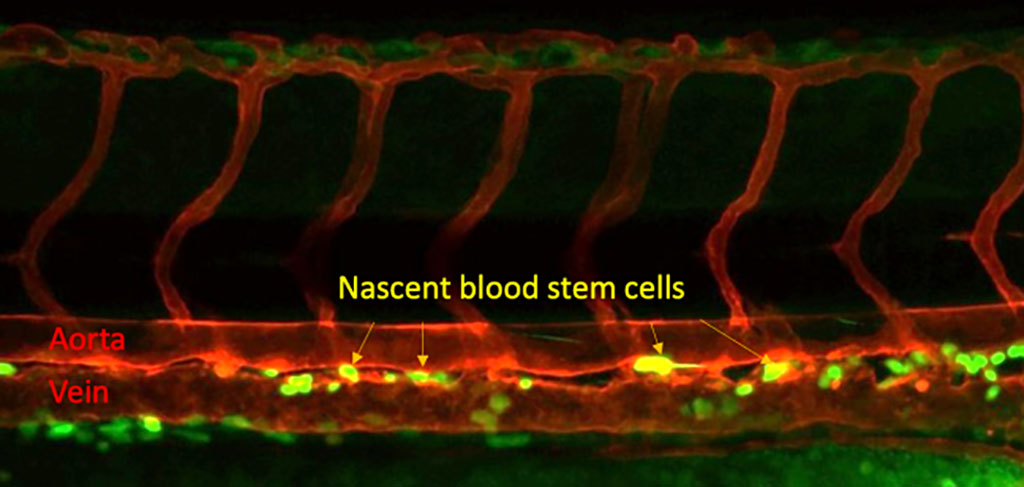
The team focused on Nod1 by examining data from human embryos and conducting studies on zebrafish, which share a significant portion of their genetic makeup with humans. They observed that the formation of blood stem cells corresponded with the levels of Nod1, as they manipulated its activity. Further experiments with human induced pluripotent stem cells, adult cells reprogrammed to an embryonic stem cell-like state, reinforced the importance of Nod1 in blood development. The absence of Nod1 led to reduced blood production, similar to the results observed in zebrafish.
Understanding Nod1's critical role in blood stem cell development is a significant step forward for scientists aiming to create a method to produce blood stem cells from human samples. This breakthrough could lead to a transformative new treatment for patients with blood disorders, allowing them to receive transfusions of blood stem cells derived from their own tissues. This approach could potentially eliminate the risks associated with graft-versus-host disease, a severe complication that occurs when the body's immune system attacks the transplanted cells. The research team continues to unravel the intricate process of blood stem cell development, focusing on the timing and expression of various signals crucial for creating a viable method for generating blood stem cells.
“My group at Iowa State University will continue working towards a life without blood disorders. I believe our investigations will pave the road to finally create therapeutic-grade blood stem cells to cure blood disorder patients,” said Raquel Espin Palazon, an assistant professor of genetics, development and cell biology at Iowa State University who led the research team.
Related Links:
Iowa State University














