Five Methods Evaluated for Constrictive Tuberculous Pericarditis Diagnosis
Posted on 24 May 2022
Constrictive pericarditis is a rare and serious disease that accounts for approximately 0.5%–2% of all heart diseases. It results in decreased pericardial compliance and can severely affect the diastolic filling function of the heart, mainly as a symptom of right heart failure, such as multiple plasma chamber effusions and edema.
Constrictive pericarditis has a poor prognosis, and pericardiectomy is the primary treatment of choice. It has several etiologies, including infection (e.g., tuberculosis [MTB], viral infection, and bacterial infection), malignancy, or radiation therapy. MTB is the most common etiology of constrictive pericarditis in developing countries.
Clinical Diagnosticians at the Zhejiang University School of Medicine (Hangzhou, China) reviewed the case histories of patients with suspected constrictive tuberculous pericarditis (TBP) hospitalized between June 1, 2019 and June 31, 2021, who underwent five tests using pericardial tissue. Fresh, diseased pericardial tissue collected during pericardial dissection was used to perform the five tests. A total of 69 patients were included.
Ground pericardial tissue specimens were centrifuged at 3000 g for approximately 15 minutes. The treated deposits were examined by smear microscopy using Auramine O fluorescent dye and stained with Ziehl–Neelsen for confirmation (AFB). Lowenstein–Jensen solid medium and liquid culture medium BACTEC MGIT 960 Mycobacteria Culture System (BD Diagnostic Systems, Sparks, MD, USA) were used for MTB culture.
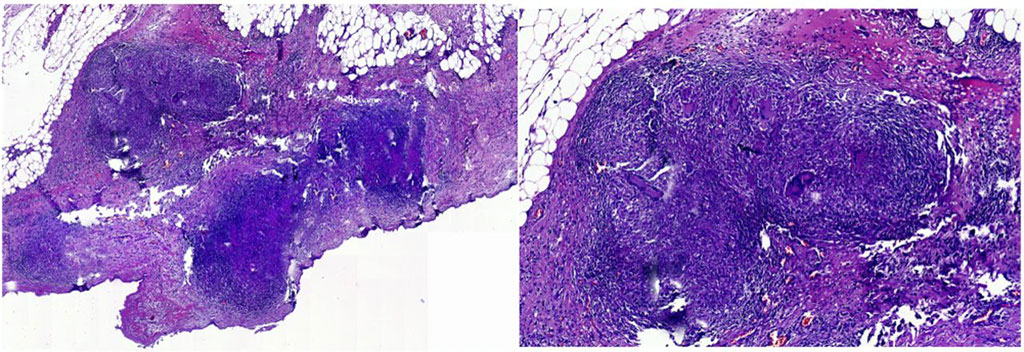
The CapitalBio Mycobacterium RT-PCR detection kit (CapitalBio Technology Inc., Beijing, China) provided simultaneous screening of MTB and nontuberculous mycobacteria (NTM) infections. It employs duplex fluorescence RT-PCR and TaqMan probe technology to detect both MTB and NTM infections in one test. The Xpert MTB/RIF assay (Cepheid, Sunnyvale, CA, USA) was also included for comparision. Histological sections were subjected to pathological examination and anti-acid staining by an experienced pathology professional.
The investigators reported that the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and AUC of AFB smear were 7.3%, 100.0%, 100.0%, 21.5%, and 0.54, respectively. Those of culture were 23.6%, 100.0%, 100.0%, 25.0%, and 0.62, respectively. Those of Xpert MTB/RIF were 52.7%, 100.0%, 100.0%, 35.0%, and 0.76, respectively. Those of CapitalBio assay were 50.9%, 100.0%, 100.0%, 34.2%, and 0.75, respectively. Those of pathology were 92.7%, 92.9%, 98.1%, 76.5%, and 0.93, respectively.
The authors concluded that the diagnosis of constrictive TBP remains challenging. The validity of AFB smear and MTB culture using pericardial tissues remains low. NAATs can provide diagnostic efficacy for TBP, but the efficacy is moderate. The CapitalBio assay and Xpert MTB/RIF could be considered similar for diagnosing TBP. The role of pathology in the diagnosis of constrictive TBP cannot be ignored, considering that pathology showed the best diagnostic accuracy among the five tests. The diagnostic accuracy of the same test is similar in acute or subacute TBP and chronic TBP. The study was published on April 13, 2022 in the International Journal of Infectious Diseases.
Related Links:
Zhejiang University School of Medicine
BD Diagnostic Systems
CapitalBio Technology Inc
Cepheid













