Clostridioides difficile Contamination Uncovered in Clinical Lab
By LabMedica International staff writers
Posted on 01 Aug 2019
Clostridioides (formerly Clostridium) difficile infection is one of the most common hospital-acquired (nosocomial) infections and is an increasingly frequent cause of morbidity and mortality among older adult hospitalized patients. C. difficile is a spore-forming, Gram-positive anaerobic bacillus that produces two exotoxins: toxin A and toxin B.Posted on 01 Aug 2019
C. difficile colonizes the human intestinal tract after the normal gut flora has been disrupted (frequently in association with antibiotic therapy) and is the causative organism of antibiotic-associated diarrhea and pseudomembranous colitis. C. difficile infection has traditionally considered to be transmitted predominantly within healthcare settings. C. difficile is not recognized as a pathogen that presents a risk of laboratory acquisition.
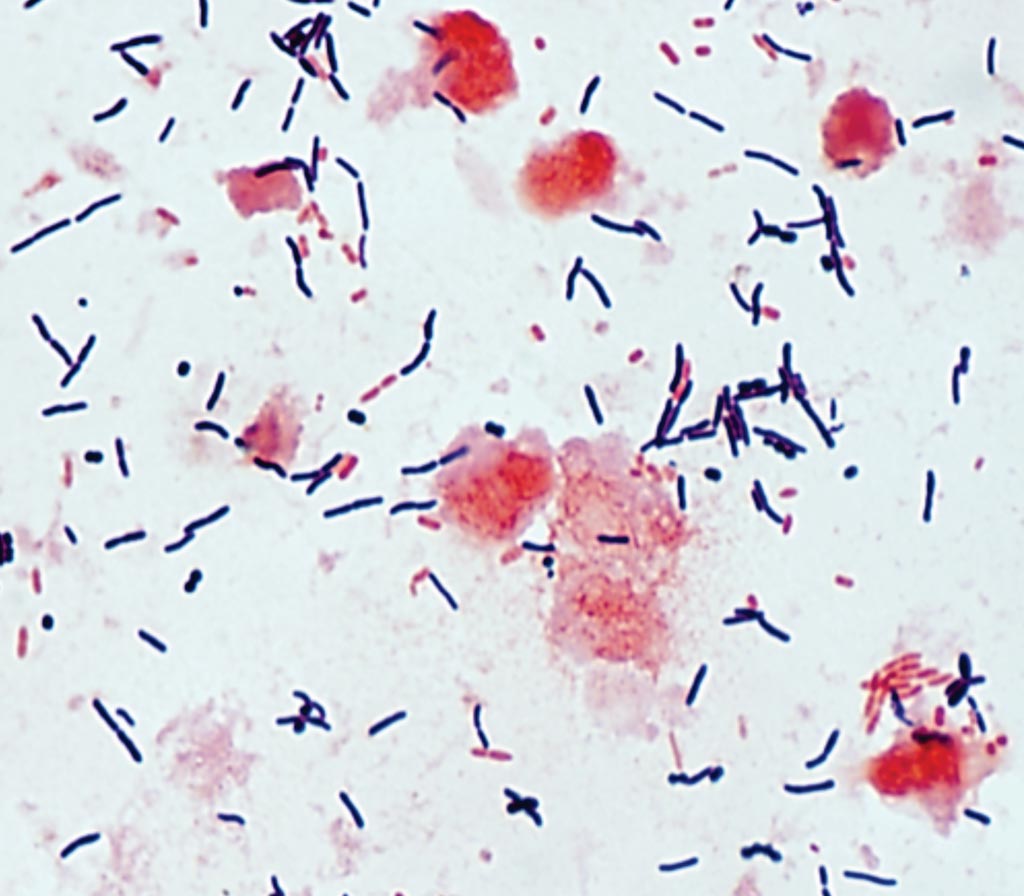
Image: A photomicrograph of Gram stain of toxigenic Clostridioides difficile from a stool sample (Photo courtesy of the University of Washington).
A team of scientists collaborating with the staff at the Hospital General Universitario Gregorio Marañón (Madrid, Spain) screened laboratory surfaces for C. difficile. Samples were taken in areas that handle C. difficile isolates (high-exposure areas), areas adjacent to high-exposure HE areas or those processing fecal samples (medium exposure areas), and areas that do not process fecal samples or C. difficile isolates (low exposure areas). They also examined C. difficile carriage (hands/rectal samples) of laboratory workers.
The team collected a total of 140 environmental samples from two high-exposure areas (n = 56), two medium exposure areas (n=56), and two low exposure areas (n = 28). Overall, 37.8% (37/98) of surfaces were contaminated with C. difficile, and 17.3% (17/98) with toxigenic C. difficile. High-exposure areas were significantly more contaminated with toxigenic C. difficile than low exposure areas (38.1% [16/42] versus 0.0% [0/14]) and medium exposure areas (38.1% [16/42] versus 2.4% [1/42]). Hands were colonized with toxigenic C. difficile in 11.8% (4/34) of cases. They found no rectal carriage of C. difficile.
The authors concluded that they had found a significant proportion of laboratory surfaces to be contaminated with toxigenic C. difficile, as well as hand colonization of laboratory personnel. They recommend specific control measures for high-risk areas and laboratory personnel working in these areas. The study was published on July 5, 2019, in the journal Clinical Microbiology and Infection.
Related Links:
Hospital General Universitario Gregorio Marañón









 (3) (1).png)




