Certain Bacteria Strains Associated with Diabetic Wounds
By LabMedica International staff writers
Posted on 01 May 2019
About 10% of Americans have been diagnosed with diabetes, and one quarter of these patients will develop a wound that does not heal. In the worst case outcome, which occurs in up to 25% percent of these wound-developing patients, the wounds will require an amputation.Posted on 01 May 2019
Many patients who develop these ulcers may not notice the initial signs, since the high blood glucose of diabetes can lead to a lack of feeling and deformation of the feet. As a result, patients with diabetes commonly develop foot ulcers that may go unnoticed over time. The mortality rate associated with diabetic foot ulcers is equivalent to that of breast cancer and prostate cancer combined, higher than 70% when they lead to amputation.
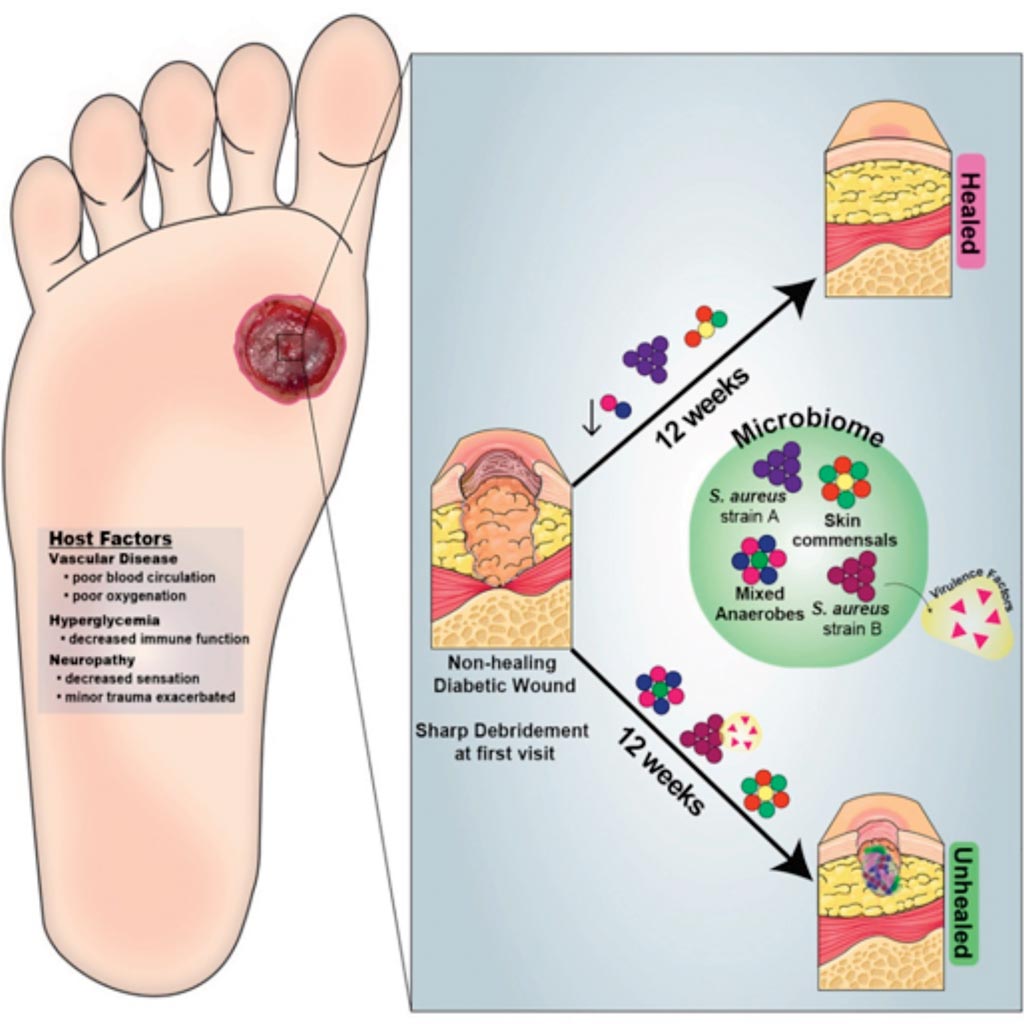
Image: A graphic representation of Strain- and Species-Level Variation in the Microbiome of Diabetic Wounds Is Associated with Clinical Outcomes and Therapeutic Efficacy (Photo courtesy of the University of Pennsylvania).
Scientists at the University of Pennsylvania School of Medicine (Philadelphia, PA, USA) and their colleagues investigated the role of colonizing microbiota in diabetic wound healing, clinical outcomes, and response to interventions, and conducted a longitudinal, prospective study of patients with neuropathic diabetic foot ulcers (DFU). Metagenomic shotgun sequencing revealed that strain-level variation of Staphylococcus aureus and genetic signatures of biofilm formation were associated with poor outcomes.
Cultured wound isolates of S. aureus elicited differential phenotypes in mouse models that corresponded with patient outcomes, while wound “bystanders” such as Corynebacterium striatum and Alcaligenes faecalis, typically considered commensals or contaminants, also significantly impacted wound severity and healing. Antibiotic resistance genes were widespread, and debridement, rather than antibiotic treatment, significantly shifted the DFU microbiota in patients with more favorable outcomes. These findings suggest that the DFU microbiota may be a marker for clinical outcomes and response to therapeutic interventions.
Elizabeth A. Grice, PhD, an associate professor of Dermatology and the lead author of the study, said, “While wounds don't receive the attention of other diseases, they're incredibly common, and our study increases our understanding of how microbes impair or promote healing. It is possible there are bacteria that actually benefit the wound, and we can use what we learned in this study to develop new treatment strategies for non-healing wounds. We hope this study will eventually help identify patients at risk for bad outcomes and lead to treatment innovations that these patients desperately need.” The study was published on April 18, 2019, in the journal Cell Host and Microbe.
Related Links:
University of Pennsylvania School of Medicine