Metagenomic Sequencing Can Diagnose Cases of Meningitis
By LabMedica International staff writers
Posted on 01 May 2018
Subacute and chronic meningitis are diagnostically challenging given the wide range of potential infectious, autoimmune, neoplastic, paraneoplastic, parameningeal, and toxic causes. Securing a final diagnosis can require weeks or months of testing or remain unsolved, necessitating empirical treatment approaches that may be ineffective or even harmful.Posted on 01 May 2018
Unlike traditional testing for specific microbes or categories of infection, metagenomic next-generation sequencing (mNGS) of cerebrospinal fluid (CSF) or brain tissue screens for nearly all potential central nervous system (CNS) infections and can identify novel or unexpected pathogens. However, mNGS data require careful analysis to determine which, if any, of the identified microbes represent a true pathogen rather than environmental contamination.
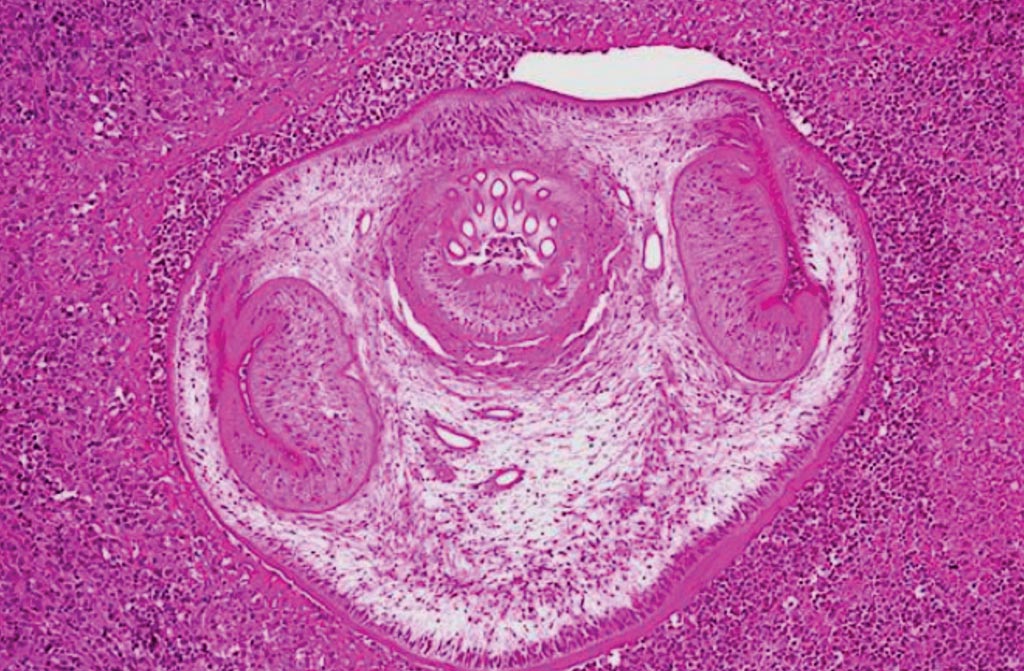
Image: A photomicrograph of a brain tissue specimen revealed the presence of hooklets in a case of cysticercosis, an infection due to the ingestion of eggs of a pork tapeworm, Taenia solium (Photo courtesy of the University of Pennsylvania Medical Center).
A large team of scientists led by those at University of California, San Francisco (San Francisco, CA, USA) enrolled seven patients who were recruited between September 2013 and March 2017 as part of a larger study applying mNGS to biological samples from patients with suspected neuroinflammatory disease. The seven participants enrolled in the present study had subacute or chronic leptomeningitis with or without encephalitis.
The team performed metagenomic next-generation sequencing on total RNA extracted from surplus CSF (250-500 μL), and one participant also had mNGS performed on total RNA extracted from snap frozen surplus tissue (<50 mg) obtained from a lumbar meningeal biopsy. Paired-end sequences of 125 to 150 base pairs were analyzed using a previously described rapid computational pathogen detection pipeline consisting of open-source components.
To distinguish putative pathogens from contaminating microbial sequences derived from skin, collection tubes, laboratory reagents, or the environment, a composite background model of metagenomic data was used. This model incorporated 24 water control samples and 94 CSF samples from patients with noninfectious diagnoses, including 21 patients with chronic meningitis with or without encephalitis.
The seven participants ranged in age from 10 to 55 years, and three (43%) were female. A parasitic worm, Taenia solium in two participants, a virus (HIV-1), and four fungi: Cryptococcus neoformans, Aspergillus oryzae, Histoplasma capsulatum, and Candida dubliniensis were identified among the seven participants by using mNGS.
The authors concluded that diverse microbial pathogens were identified by mNGS in the CSF of patients with diagnostically challenging subacute or chronic meningitis, including a case of subarachnoid neurocysticercosis that defied diagnosis for one year, the first reported case of CNS vasculitis caused by Aspergillus oryzae, and the fourth reported case of C. dubliniensis meningitis. The study was published on April 16, 2018, in the journal JAMA Neurology.
Related Links:
University of California, San Francisco