Vaginal Infection Increases Risk of Fetal Membrane Rupture
By LabMedica International staff writers
Posted on 05 Feb 2018
Posted on 05 Feb 2018
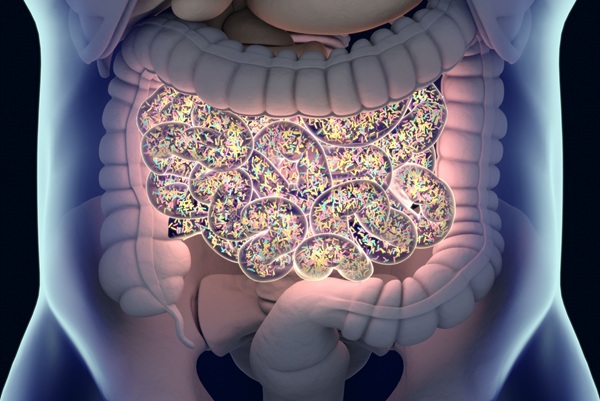
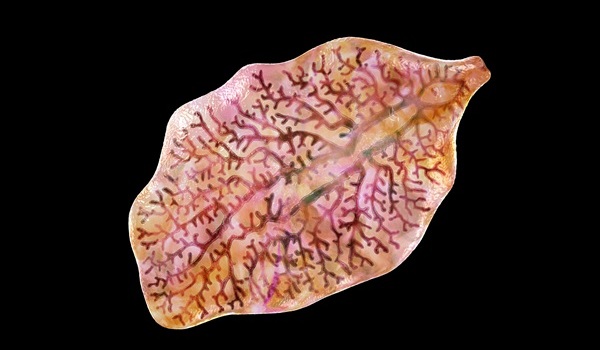
Preterm pre-labor rupture of the fetal membranes (PPROM) precedes 30% of preterm births and is a risk factor for early onset neonatal sepsis. As PPROM is strongly associated with ascending vaginal infection, prophylactic antibiotics are widely used.

Image
It has been hypothesized that colonization of the vagina with pathogenic bacteria activate the local and upper (cervical and fetal membrane) innate immune system driving an inflammatory cascade that leads to remodeling and disruption of membrane architecture and premature rupture.
Scientists at the Imperial College London (London, UK) and their colleagues performed a prospective cohort study whereby 250 women with and without risk factors for preterm birth were recruited between 8 and 12 weeks from the preterm surveillance at antenatal clinics between January 2013 and August 2014. A second cohort of 87 was recruited upon presentation with ruptured membranes between October 2013 and June 2015.
DNA extraction from vaginal swabs and confirmation of DNA integrity by polymerase chain reaction (PCR) amplification was performed. Sequencing was performed using an Illumina MiSeq platform (Illumina Inc, San Diego, CA, USA). The total number of 16S rRNA gene copies per swab was measured as a representation of the total bacterial load. A bacterial DNA template was used for broad coverage quantitative real-time PCR using the BactQUANT method.
The scientists reported that in contrast to pregnancies delivering at term, vaginal dysbiosis characterized by Lactobacillus spp. depletion was present prior to the rupture of fetal membranes in approximately a third of cases and persisted following membrane rupture (31%). Vaginal dysbiosis was exacerbated by erythromycin treatment (47%) particularly in women initially colonized by Lactobacillus spp. Lactobacillus depletion and increased relative abundance of Sneathia spp. were associated with subsequent funisitis and early onset neonatal sepsis. Further analysis identified 20 genera positively associated with membrane rupture including Prevotella, Staphylococcus, Aerococcus and Streptococcus spp., and a negative association with Lactobacillus spp.
The authors concluded that their data show that vaginal microbiota composition is a risk factor for subsequent PPROM and is associated with adverse short-term maternal and neonatal outcomes. This highlights vaginal microbiota as a potentially modifiable antenatal risk factor for PPROM and suggests that routine use of erythromycin for PPROM be re-examined. The study was published on January 24, 2018, in the journal BMC Medicine.