New Methods Developed to Diagnose TB and HIV
By LabMedica International staff writers
Posted on 15 Nov 2017
The bacteria responsible for tuberculosis (TB) can lurk in a person's lung tissue for decades before producing active, infectious TB disease and it is estimated that a third of the global population may have such dormant infections, with 5% to 10% progressing to active disease. Detecting TB is notoriously challenging.Posted on 15 Nov 2017
While tuberculosis can be cured, this requires that patients adhere to a strict drug regimen for months, despite common side effects, and multi-drug resistant TB bacteria are becoming more common. Current diagnostic methods can take a long time and poorly detect TB in certain types of patients, including children and patients with HIV infections, making it difficult to determine who needs to be treated and when they have been cured of disease.
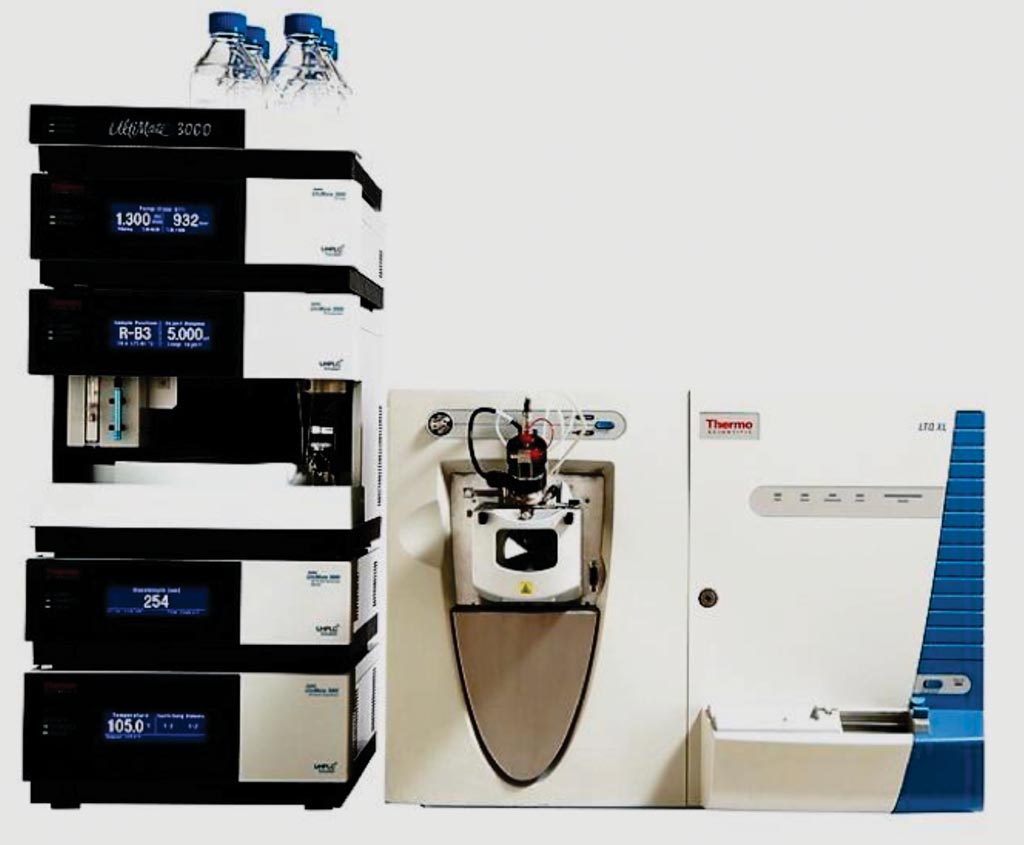
Image: The LC UltiMate 3000 high performance liquid chromatography (HPLC) system coupled with an LTQ Velos Pro mass spectrometry system (Photo courtesy of Thermo Fisher Scientific).
Scientists at Arizona State University (Tempe, AZ, USA) applied nanotechnology-based approaches to detect TB proteins in patient blood samples to improve disease detection. Unlike existing methods that attempt to identify bacteria or bacterial DNA in sputum or tissue samples, their two methods measure TB-derived factors released into the blood only during active TB infections and provide a measure of the number of active TB bacteria in the patient.
The team examined HIV-positive adults enrolled in the Houston Tuberculosis Initiative, a large TB screening and surveillance study which ran from October 1995 to September 2004.The investigators performed their analysis using the PRM Mode on a nano-LC UltiMate 3000 high performance liquid chromatography (HPLC) system coupled with an LTQ Velos Pro mass spectrometry system. By measuring the TB protein 10 kDa culture filtrate antigen (CFP-10) in the blood of HIV-infected subjects, the group detected 85% percent of all TB cases and 67% of culture-negative TB cases, much better than the best available molecular test, which is reported to detect only 9% of culture-negative TB cases in HIV-infected patients.
The authors concluded that their study indicated that serum CFP-10 measurement can greatly improve TB diagnosis rates in HIV/TB-co-infected patients, who are diagnosed with reduced efficiency by current TB diagnostics. Improved TB diagnosis is a major unmet need for HIV-infected patients, as undiagnosed and untreated TB is a major cause of excess morbidity and mortality. The study was published on November 1, 2017, in the journal BMC Medicine.
Related Links:
Arizona State University









 (3) (1).png)